Top Links
Journal of Vascular Health and Surgery
Variation in Anatomy Complicating Exposure for Abdominal Aortic Aneurysm
Copyright: © 2018 Wehbe MR. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Related article at Pubmed, Google Scholar
An 82 years old male presented to our clinic almost 11 years after initial incidental diagnosis of a 5cm abdominal aortic aneurysm (AAA) after which he was lost to follow up. He had stable vital signs and was found to have a large pulsatile mass upon abdominal examination. His laboratory tests were within normal limits. CT scan of the abdomen and pelvis showed a juxtarenal 10 cm AAA not extending to the iliac bifurcation. The patient’s history was relevant for hypertension on treatment and coronary artery disease with recent stenting for which he was on dual antiplatelet therapy.
Due to the aneurysm’s short angulated neck, and unusual very short common iliac arteries (2.5cm in length) endovascular repair was considered not to be his best option. The patient was planned for elective open transabdominal repair. During midline exploration the transverse, descending and sigmoid colon were the most anterior structures; and the left colon was not attached as normally to the line of Toldt. All the small bowel was found in a peritoneal sac posterior to the mesocolon, in a middle and left postero-lateral abdominal position. A transmesocolic or and Standard left visceral rotation approach was deemed unsafe without compromise of bowel vascularity. The aneurysm was treated using a right medial visceral rotation and mobilization of sigmoid and ascending colon and Kocherization of the duodenum. Fortunately a tube graft was feasible, since the exposure and control of the left iliac system was more difficult through that exposure. This case went uneventful after that. The diagnosis after intraoperative findings and image reviews was transmesocolic hernia (Figure 1).
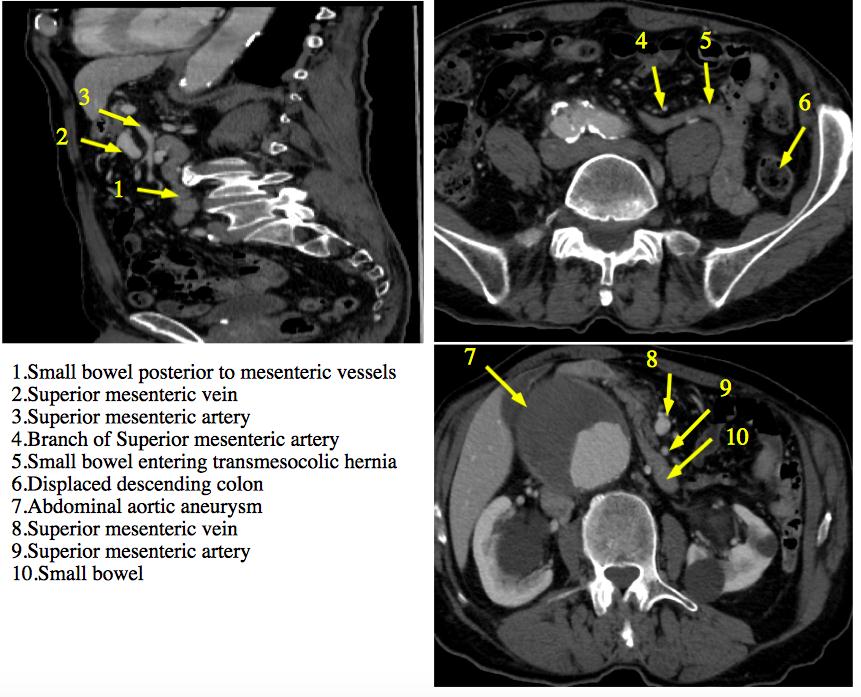 |
Figure1 |






































