Top Links
Journal of Case Reports and Studies
ISSN: 2348-9820
Accidental Hypothermia in the Upper Midwest: A Dual Case Report Comparison
Copyright: © 2016 Jacobson E. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Related article at Pubmed, Google Scholar
Accidental hypothermia is a potentially life-threatening situation that involves a debilitated patient and is a result of environmental exposure. In rural and isolated areas, rapid transport of a patient for definitive care is of extreme importance. Recently, an air ambulance service in the Upper Midwest encountered two similar patients within a 40 day period that experienced strikingly different outcomes. This experience brought to light the lack of a regional protocol for the management of accidental hypothermia, and has subsequently incited the development of a detailed management plan. The goal of the protocol is to unify the approach and standardize the process of hypothermia management in critical access hospitals. Of key importance in relation to the presented cases is the rapid transfer of hypothermic patients treated with CPR to a center capable of cardiopulmonary bypass.
Keywords: Accidental hypothermia; Air ambulance; Cardiopulmonary bypass; Case comparison; Regional hypothermia protocol
List of Abbreviations: ACLS: Advanced cardiac life support; AHA: American Heart Association; BPM: Beats per minute; CPR: Cardiopulmonary resuscitation; ECMO: Extracorporeal membrane oxygenation; oC: degrees Celsius; oF: degrees Fahrenheit; EMR: Electronic medical record; ED: Emergency department; EMS: Emergency medical services; ET: Endotracheal; mEq/L: Milliequivalents per liter; mg/dL: Miligrams per deciliter; mm Hg: Millimeters mercury; mmol/L: Millimols per liter
Accidental hypothermia is the result of environmental exposure, often prolonged, in an incapacitated or inadequately prepared person. The Center for Disease Control reported an average of 1301 deaths by excessive natural cold per year in the period of 1999-2011 [1]. Hypothermia is categorized by initial core temperature, and classified as mild (35-32 oC), moderate (32-28 oC), or severe (<28 oC) [2,3].
Harsh temperatures in the winter months of the Upper Midwest provide for a substantial risk of severe accidental hypothermia. The rural nature of the area provides for significant barriers to healthcare resources. Indirect roadways, extended distances to definitive care centers, and an inability of local care centers to be able to manage severe emergency and trauma are challenges often faced in providing the patient with the best possible care.
Air ambulance services are located among the communities to provide rapid transport. These services, with locations throughout the Upper Midwest, utilize fleets of rotor and fixed wing aircraft able to rapidly launch to the scene of an emergency or referring facility [4]. One particular air ambulance crew was presented with two similar cases of accidental hypothermia within a 40 day period that resulted in strikingly different outcomes.
Information regarding both cases featured in this report was gathered from the EMR. This includes physician notes, nursing notes, radiology reports, and lab results from two participating institutions as well as scanned documents from EMS services. Supplemental information was obtained via conferences with first-hand participants in patient care. The regional hypothermia protocol was obtained directly from the Trauma Services Department at Sanford Health Fargo. The compiled information was drafted into this manuscript by the listed authors. The need for Institutional Review Board approval for this case report was waived by the participating institutions.
Patient A was found unresponsive after an unknown period of exposure, having experienced atmospheric temperatures as low as -14.0 oC (wind-chill -19.8 oC). The patient, a 20-year-old-female smelling strongly of alcohol, was found wearing only thin leggings, a shirt that exposed her midsection, and one boot on her right foot, with areas of full thickness frostbite to her left foot. Her medical history included an allergy to ciprofloxacin and sulfa drugs. Initial vitals presented with a heart rate of 76 bpm and a blood pressure of 66/42 mm Hg. The patient alternated between sinus rhythm and atrial fibrillation.
EMS transported the patient to the local hospital, a rural primary care center with limited surgical and critical care capabilities, arriving in the ED 19 minutes after dispatch. The patient was intubated, and shortly after a code was initiated due to lack of palpable pulse and auscultated heart rhythm. CPR was started using a LUCAS automated compression device. After administration of epinephrine and one defibrillation attempt, the LUCAS was removed to allow a chest x-ray. Manual compressions then resumed, and seven minutes later the patient established ventricular fibrillation. A large amount of blood was also noted to be coming out of the ET tube.
Initial temperature was documented at 23.6 oC. The anatomical site and method of temperature measurement was not documented. Cardiopulmonary bypass was not available at this center, so other rewarming techniques were utilized. Rewarming was initiated with warm fluid infusion, warm water irrigation through a Foley catheter, gastric lavage through nasogastric tube, pleural lavage through bilateral chest tubes, and external warming blankets. Foley return was noted to be pink-tinged.
Lab results showed a blood potassium level normal at 4.6 mEq/L. Arterial blood gas showed a mixed respiratory/metabolic acidosis, with pH = 6.82, pCO2 = 57 mm Hg, pO2 = 75 mm Hg, and HCO3 = 9 mmol/L. The patient was given a total of 11 ampules of 8.4% sodium bicarbonate throughout resuscitation efforts. Lactic acid level was not obtained. Blood alcohol was 201.3 mg/dL.
One more defibrillation was attempted, again unsuccessfully. Esophageal probe was placed and the patient’s core temperature was read at 24.7 oC. The LUCAS device was reapplied after a period of 50 minutes of manual compressions, and epinephrine was again administered.
The air ambulance service was dispatched for transport shortly after the patient’s arrival in the ED. They were forced to utilize a fixed wing aircraft due to weather concerns, and arrived 90 minutes after the patient arrival. With the initiation of transfer complicated by numerous ongoing procedures and delayed by the use of a fixed wing aircraft rather than a rotor wing aircraft, it was decided to forgo transfer and continue resuscitation efforts at the current facility.
Core temperature reached 26.7 oC via esophageal probe, and sodium bicarbonate and epinephrine were given. Defibrillation was again attempted one time, unsuccessfully. Blood transfusion was started due to the blood loss witnessed. The batteries in the automated compression device failed after three hours, and manual compressions were conducted for 38 minutes before the batteries were replaced.
Three more attempts at defibrillation proved unsuccessful. Core temperature had reached 30.7 oC via esophageal probe. Defibrillation was again unsuccessful after two more attempts, and the patient was given 300 mg amiodarone. Four hours and eight minutes post ED arrival, it was decided to cease resuscitation efforts, and the patient expired.
Patient B was found unresponsive after approximately nine hours of exposure, having experienced atmospheric temperatures as low as -5.0 oC (wind-chill -8.5 oC). The patient, a 19-year-old female with no previous medical history, was noted as wearing jeans, a tank top, and sweatshirt. She smelled strongly of alcohol. A faint pulse was estimated at 30 bpm. A cardiac monitor was applied as the patient was loaded onto the stretcher, and she was found to be in ventricular fibrillation. En route to the ED, CPR was initiated and defibrillation was attempted once, unsuccessfully.
Patient B arrived at the local hospital, the same rural primary care center with limited surgical and critical care capabilities, 21 minutes after EMS dispatch. She was intubated and started on mechanical ventilation. CPR was continued with a LUCAS automated compression device. Her initial core temperature reading was 24 oC via rectal probe. Rewarming efforts were initiated, limited by the lack of available cardiopulmonary bypass. Efforts included infusion of warm normal saline under pressure through bilateral intravenous lines, warm water irrigation through a Foley catheter, pleural lavage through a single left chest tube, warm peritoneal lavage, warm water lavage through nasogastric tube, and application of external warming blankets.
Initial labs showed mild hypokalemia with a potassium level of 3.2 mEq/dl. Lactic acid level was high at 5.2 mmol/L. Venous blood gas showed a possible mild mixed respiratory/metabolic acidosis, with pH = 7.03, pCO2 = 69 mm Hg, pO2 = 45 mm Hg, and HCO3 = 18 mmol/L. No pharmacologic interventions were utilized. Blood alcohol level was 183.6 mg/dL.
The air ambulance service was dispatched prior to patient arrival in the ED and arrived in 15 minutes, only 47 minutes after EMS activation. During transfer preparation the patient remained in ventricular fibrillation with a core temperature of 26.6 oC via rectal probe. The patient departed the ED 48 minutes after the air ambulance arrival (95 minutes after EMS dispatch).
The patient reached a Level II trauma center via helicopter 50 minutes after departing the ED (145 minutes after EMS dispatch). Ventilation and CPR with the LUCAS device were continued throughout transport. The patient was continually suctioned throughout transfer. Core temperature reached 27.7 oC via rectal probe.
Patient B was taken directly to the operating room for an emergent median sternotomy, internal cardiac massage, placement of cardiopulmonary bypass, and core temperature rewarming. Sternotomy with cardiopulmonary bypass was performed instead of ECMO due to the unavailability of adult ECMO at this facility. She was successfully defibrillated into normal sinus rhythm. She was weaned from bypass after reaching normothermia, and taken to intensive care.
Labs drawn once sinus rhythm was restored showed normal potassium levels of 5.0 mEq/L. Arterial blood gas showed acidemia, with pH = 7.24, pCO2 = 43, pO2 = 52, and HCO3 = 18 mmol/L. Lactic acid level was high at 8.5 mmol/L. These disturbances were managed and corrected during her stay in the intensive care unit. The patient was successfully weaned from sedation post-operative day two, extubated post-operative day three, and transferred to the medical/surgical floor post-operative day four. She was fully alert and ambulatory.
The patient was discharged home post-operative day seven with no organ system dysfunction, no neurologic sequellae, and some minor second degree blistering on her abdomen, with no other injury or illness. She was seen in follow-up 18 days after discharge and reported feeling well. Vital signs, chest x-ray, and ECG were all normal. Her surgical wound and frostbite injuries were healing well. She has now made a full recovery.
The similarity between these two patients is most evident in their presentation. Both young, college-aged women, both severely intoxicated. Both were found unresponsive after a long period of exposure wearing minimal clothing. Despite Patient A withstanding colder temperatures, both had an initial temperature reading within 0.4 oC. The differences in the course of care for these two young women, resulting in death for one and full recovery for the other, has brought to light the need for a definitive management plan unique to the rural region served by our regional air ambulance services and critical access hospitals.
The main difference in these cases was the rapid transport to definitive care of a hypothermic patient treated with CPR to a center capable of performing cardiopulmonary bypass. In the case of Patient B, the air ambulance team was dispatched before the patient had even reached the local ED. They arrived 47 minutes after the initial EMS call, and the patient reached a definitive care center 145 minutes after the EMS call, where she received the appropriate care and made a full recovery.
For Patient A, air ambulance was not notified until the patient had been in the local ED for 15 minutes. Due to weather conditions, the air ambulance team did not arrive until 109 minutes after initial EMS dispatch. As mentioned, there was hesitation regarding transport due to a number of complicating factors, including the extensive interventions already in progress, bleeding complications related to her hypothermic state [5,6], and transportation concerns.
Despite these complicating factors, whether controllable or uncontrollable, it is apparent in retrospect that the benefits of transfer for cardiopulmonary bypass outweigh the risks of transport in hypothermic patients treated with CPR. The differences in the fine details of these cases have also emphasized the need for standardization of care in order to best direct management decisions. A clear protocol for resuscitation based on ACLS guidelines, a standardized method of temperature measurement, and a defined slate of blood tests to aid in prognosis are all important tools with high value for medical decision making.
The need for a standardized, directed approach to care for the hypothermic patient in a rural setting has resulted in the development of a regional protocol for the management of accidental hypothermia. The protocol’s main goal is to unify the approach and standardize the process of hypothermia management in critical access hospitals. The management plan enacts an organized team approach to provide timely and efficient external core rewarming, and promotes early transfer to a tertiary care center for the most critical patients. The approach to this is outlined as follows:
1. Rewarm to >95 oF (35 oC) at a controlled rate.
a. In moderate to severe hypothermia, goal is 2 oC/hour [7,8].
2. Prevent any recurrent cooling.
3. Limit time to definitive care.
4. Provide efficient stabilization that does not delay definitive care.
5. Initiate transfer when:
a. CPR is part of treatment.
b. Frostbite associated with the hypothermia.
c. Frozen extremity identified.
d. Trauma associated with the event.
More specific aspects of management are broken down according to severity of hypothermia based on initial core body temperature. The protocol also outlines specific actions for management of different situations, including indications for CPR, recommendations for management of cardiac arrest, management of hypotension associated with rewarming, protocols for defibrillation, management of ACLS drugs, and recommendations for laboratory tests for moderate and severe hypothermia [9,10]. These aspects of the protocol are detailed in Figure 1. Also of note is the advocated use of an esophageal probe for temperature monitoring and continuous use of an automated compression device for compressions. The recommendations of the management plan are based on current ACLS and AHA guidelines.
The lessons learned from these two cases have shed a light on the need for a definitive management plan in the treatment of accidental hypothermia in our northern region. The protocol described in this report has been implemented throughout the region, with hopes to improve patient care in cases such as these.
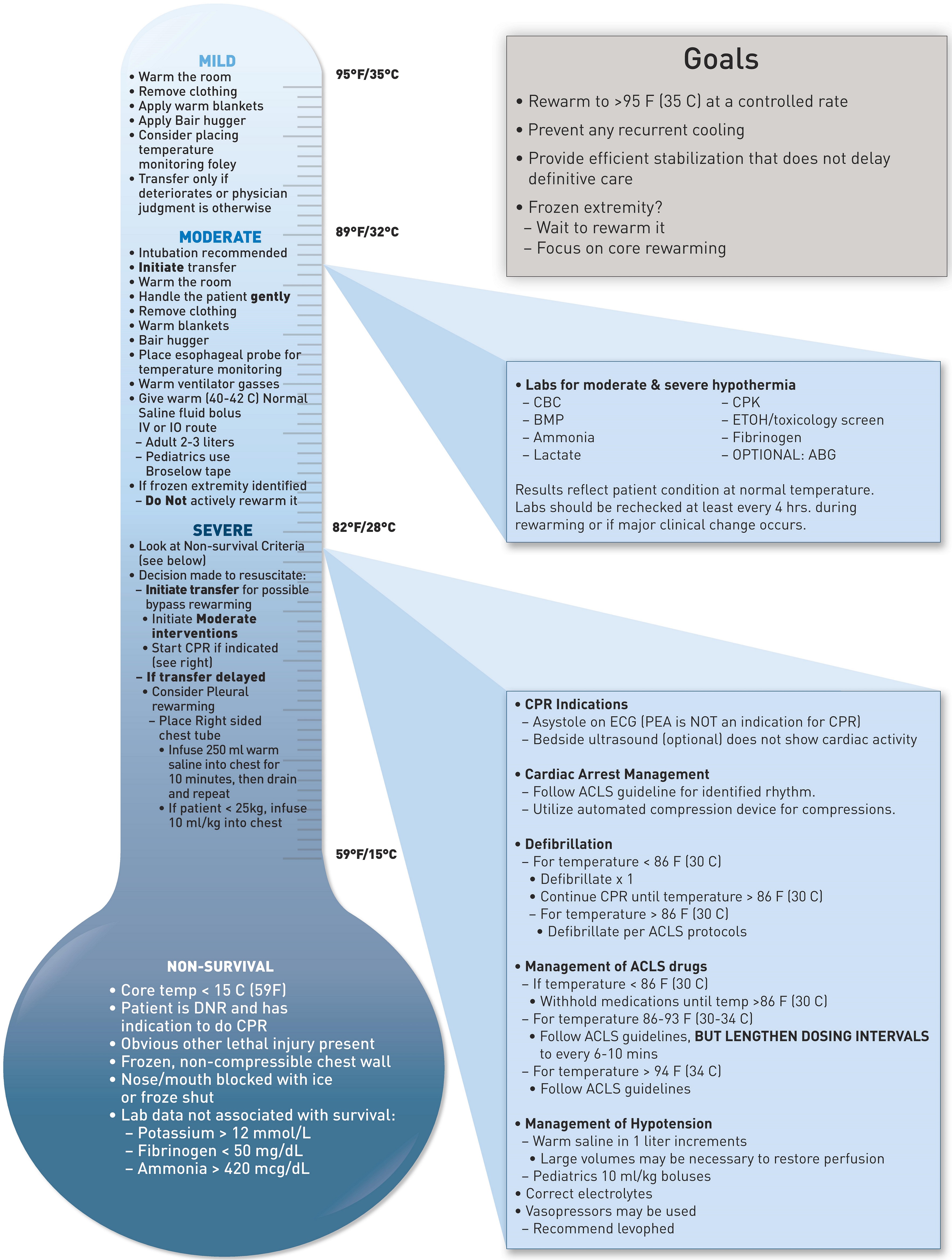 |
F = Fahrenheit, C = Celsius, IV = intravenous, IO = intraosseous, CPR = cardiopulmonary resuscitation, ml = milliliters, kg = kilograms, DNR = do not resuscitate, mmol/L = millimols per liter, mg/dL = milligrams per deciliter, mcg/dL = micrograms per deciliter, CBC = complete blood count, BMP = basic metabolic panel, CPK = creatinine phosphokinase, ETOH = ethanol, ABG = arterial blood gas, ECG = electrocardiogram, PEA = pulseless electrical activity, ACLS = advanced cardiac life support |






































