Top Links
Journal of Case Reports and Studies
ISSN: 2348-9820
Langerhans Cell Histiocytosis in a Patient with Lynch Syndrome (Hereditary Non Polyposis Colorectal Cancer)
Copyright: © 2015 Battley JE. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Related article at Pubmed, Google Scholar
A fifty three year old white female smoker with Lynch Syndrome was receiving adjuvant chemotherapy for node positive caecal adenocarcinoma. Interval investigations demonstrated a second primary gastric cancer with bilateral pulmonary nodules of indeterminate significance. Lung biopsy revealed Langerhans cell histiocytosis (LCH). Our case highlights the importance of non-malignant pathology mimicking malignancy in a patient at risk of multiple primary tumors. To our knowledge an association between Lynch syndrome and LCH has not been previously documented, we review the literature.
Abbreviations: LCH: Langerhans Cell Histiocytosis; CEA: Carcinoembryonic antigen; PET: Positron emission tomography; FDG: Fludeoxyglucose; CT: Computed tomography
We report the case of a fifty three year old white female smoker with Lynch Syndrome with a known deletion in the MutL homolog 1 (MLH1) gene. The patient is one of 14 siblings with a brother and sister diagnosed with colon cancer; she has 8 children with one son a confirmed carrier.
The patient was diagnosed with a caecal adenocarcinoma at the time of gynecological risk-reduction surgery and underwent right hemicolectomy for a pT3pN2apM0 tumour (4/22 lymph nodes positive), R0 resection, MLH1 and postmeiotic segregation increased 2 (PMS2) deficient, microsatellite unstable, B-Raf proto-oncogene, serine/threonine kinase BRAF V600 mutation testing was negative. Adjuvant chemotherapy was fragmented due to post-operative pain and poor tolerance. Serum CEA levels initially fell following surgery but plateaued and remained moderately elevated but stable, concordant with the patient's active cigarette smoking history. Due to new onset weight loss and ongoing abdominal pain an interval PET scan was arranged following the completion of 15 of a planned 30 treatments of single-agent 5-fluorouracil. This revealed increased FDG uptake in the distal stomach and right colon with mildly FDG avid bilateral centrilobular pulmonary nodules, predominantly apical, of indeterminate significance (Figure 1). No evidence of bowel recurrence was found on colonoscopy. Gastroscopy revealed an ulcerated, fungating lesion in the gastric antrum. Biopsy confirmed poorly differentiated adenocarcinoma. A repeat CT scan of the thorax, performed 6 weeks later, showed persistence of the pulmonary nodules (Figure 2). No evidence of malignancy was found on bronchoscopy, lung biopsy revealed LCH (Figure 2a), with CD1a expression, a marker of epidermal Langerhans cells (Figure 2b). No further molecular testing including other molecules of the ERK signaling pathway was performed. There was no evidence of extrapulmonary LCH. The patient reported chronic cough productive of clear sputum but otherwise denied respiratory symptoms.
The patient subsequently underwent a subtotal gastrectomy, for a perforated T4a tumour measuring 2.7cm in size with lymphovascular invasion, 6 of 27 nodes were involved. Adjuvant chemotherapy with 5-flourouracil was initiated. She has not yet received any LCH targeted therapy but remains under respiratory surveillance.
LCH is a rare disease characterized by proliferation of abnormal cells resembling epidermal dendritic Langerhans cells. According to recent findings, LCH cells exhibit a unique transcription profile that separates them from plasmacytoid and myeloid dendritic cells, but also from epidermal Langerhans cells, indicating a distinct dendritic cell entity [1].
The normal physiological function of Langerhans cells is the processing and presentation of skin-derived antigens. LCH is part of a spectrum of histiocytic disorders categorized by the Histiocyte Society into group I (LCH), group II (non-Langerhans, mononuclear phagocyte histiocytic proliferations) and group III (malignant histiocyte disorders) [2]. Group I disorders can be further classified according to the extent of organ system involvement. LCH may involve a single organ (single-system LCH), which may be unifocal or multifocal, or multiple organs (multisystem LCH), which can be disseminated.
Adults are likely to have isolated pulmonary LCH (PLCH), however extrapulmonary involvement is seen in up to 30% of cases [3,4]. Adult PLCH occurs almost exclusively in smokers; it is now recognized as a form of smoking-related interstitial lung disease and can be complicated by pulmonary fibrosis and pulmonary hypertension.
The incidence of adult LCH is estimated to be one to two cases per 1 million population [5] however as most studies are nonpopulation based, the true incidence is unknown. A German study of 58 adults with LCH reported an average age of 43.5 years, 66% were women, the pulmonary system was most frequently involved, and however almost one-third of the patients had multisystem disease. Almost 90% of patients were smokers or ex-smokers [6].
Whether the proliferation of LCH cells is the result of an immunologic stimulus or results from a neoplastic transformation remains controversial. Recent studies demonstrate that the majority of patients with LCH demonstrate BRAF and other retrovirus associated sequence oncogene (RAS) pathway mutations. Biopsy samples of LCH have shown that approximately 60% demonstrate mutations in the V600E portion of the BRAF oncogene reported in other malignancies including malignant melanoma. This may have implications for the use of targeted therapy and clinical trials using BRAF inhibitors in V600E mutated tumours including LCH are in progress. Other targeted therapies under investigation include tyrosine kinase inhibitors.
Evidence to guide the optimal treatment of adult LCH is limited due to a lack of clinical trials. Patients with PLCH may recover spontaneously or remain stable with or without smoking cessation or treatment. Some patients have been reported to respond to cladribine therapy. In adults with LCH with extensive pulmonary destruction lung transplantation may be required [7].
In the present case the presence of bilateral lung nodules in a patient with a history of two malignancies raised the issue of metastatic lung disease, which would have impacted on the decision to pursue potentially curative surgery to the primary lesion. This case highlights the importance of non-malignant pathology mimicking malignancy in a patient at risk of multiple primary tumors. To our knowledge, this is the first report of concurrent Lynch syndrome and LCH.
 |
| Figure 1: CT thorax demonstrating a number of ill-defined nodules including a) ground glass centrilobular nodules b) small nodules with tiny cavities and c) small ill-defined more solid nodules |
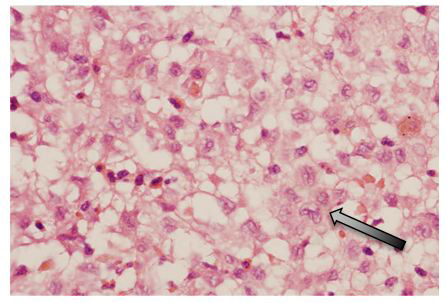 |
| Figure 2a [H/E]: Langerhans cells with folded nuclei and abundant cytoplasm (arrow) admixed with eosinophils |
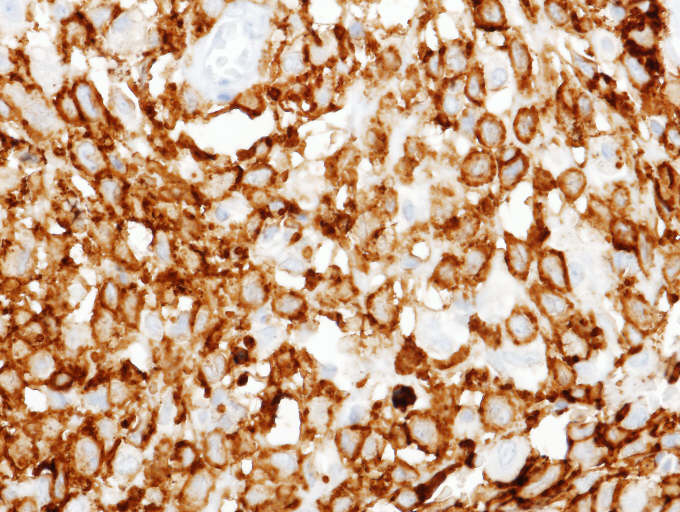 |
| Figure 2b: CD1a positive Langerhans cells |






































