Top Links
Journal of Hematology and Blood Disorders
ISSN: 2455-7641
Evaluation of Prognostic Factors and Survival Results in Pediatric Hodgkin’s Lymphoma-single center experience from Eastern Black Sea Region of Turkey
Copyright: © 2016 Kandaz M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Related article at Pubmed, Google Scholar
Objective: Study clinical features and treatment results of Pediatric Hodgkin's Lymphoma patients and investigate prognostic factors affecting survival.
Materials and Methods: Data of 44 Hodgkin's Lymphoma patients (15 females, 29 males) below 16 years of age [mean age 10.4 ± 4.2 (3-16)] treated and monitored in our institution between 1996 and 2015 was studied retrospectively.
Results: 50% of the patients had early stage (stage I-II) of the disease. The most common histological type was mixed cellular Hodgkin's lymphoma (MCHL). All patients received chemotherapy. After chemotherapy, involved field radiotherapy was administered to all patients. Median survival time was 164.32±13.8 months and 1-, 3-, 5- and 10-year survival rates were 96%, 91.8%, 88.3% and %87.9, respectively. In univariate analysis, stage (p<0.005) and ECOG performance score (p<0.0001) were found to be variables with effects on overall survival. In multivariate analysis, only ECOG performance score (p<0.003) was found to be statistically significant.
Conclusion: Although our treatment results are similar to those of other treatment centers, we will be able to contribute more to clinical features and treatment results of pediatric Hodgkin's lymphoma patients, with higher number of patients.
Keywords: Pediatric Hodgkin's lymphoma; Patient’s characteristics; Chemotherapy; Radiotherapy; Prognostic factors; Survival
Hodgkin's lymphoma constitutes 1% of all cancers and 25 to 40 % of lymphomas [1]. Lymphomas comprise 25% of childhood cancers and they are the second most common group of cancer after leukemias. It peaks twice with one at the second decade and one at the fifth decade [2]. It is observed at an early age especially in developing countries, however, it is observed after 55 years of age in developed countries. Its incidence at an early age is also high in Turkey [2,3]. Its incidence below 15 years of age is 5-7/1000000. In its etiology, autoimmune factors, genetic, and certain virus (such as EBV) infections are held responsible [4].
Among oncological diseases, Hodgkin's lymphoma has a high cure rate. Overall survival and disease-free survival rates have increased considerably especially in recent years by combined use of chemotherapy (CT) and radiotherapy (RT) in the treatment protocol.
The aim of this study was to determine the outcomes of our patients who presented with favorable risk early-stage Hodgkin lymphoma, unfavorable risk early-stage Hodgkin lymphoma and advanced stage Hodgkin lymphoma that were treated either with chemotherapy plus radiotherapy and prognostic factors affecting treatment response and survival.
Data of 44 Hodgkin's Lymphoma patients aged ≥3 - ≤16 years diagnosed, treated and currently on follow-up in our institution between 1996 and 2015 was studied retrospectively. From patient files; sex, age, complaints, histology, stage, region of involvement of lymph node, presence of B symptoms ( fever > 38 oC, night sweats, and more than 10% weight loss in the last six months), whether there is any extranodal involvement, splenic involvement and bone marrow involvement or not were all noted. Eastern Cooperative Oncology Group (ECOG) scale was used for performance status of the patients. Cotswolds Modification of Ann Arbor staging system was applied during staging. In addition, patients were classified into early stage (stage I-II) favorable group (favorable factors for stage I-II disease: no bulky mediastinal or <10 cm disease, erythrocyte sedimentation rate (ESR)<50, ≤3 sites of disease), early-stage (stage I-II ) unfavorable group (unfavorable factors for stage I-II disease: bulky mediastinal or ≥10 cm disease, B symptoms, ESR >50, >3 sites of disease) and advanced stage (stage III-IV) disease according to risk factors, including whether a patient has bulky disease, extranodal involvement, high sedimentation (if the patient has B symptom, ≥30; if not, ≥50 ) and ≥ 3 involved areas. The presence of lymphadenopathy that was 1/3 greater than the widest intrathoracic diameter on the T5-6 level in plain lung radiography and peripheral lymphadenopathy whose largest diameter was ≥ 5 cm were considered to be bulky disease. The patients’ hemoglobin (Hb), ESR and lactate dehydrogenase (LDH) levels were recorded at the time of first admission. Applied treatments (chemotherapy, radiation therapy and bone marrow transplantation) were recorded. Treatment responses were evaluated by using imaging modalities as Computerized tomography and PET-CT, where appropriate.
All patients received ABVD (Adriamycin (25 mg/m2 on 1st and 15th days), Bleomycin (10 mg/m2 on 1st and 15th days), Vinblastine (6 mg/m2 on 1st and 15th days) or Vincristine (1.5 mg/m2 on 1st and 15th days), Dacarbazine (375 mg/m2, on 1st and 15th days)) protocol as CT (18 patients (41%) received 2 doses, 18 patients (%41) 4 doses, and 8 patients (%18) 6 doses).
RT (15-41.4 Gy) was administered to 44 patients after CT. The 3 dimensional conformal radiotherapy (3DRT) techniques were used. The clinical target volume (CTV): the area where the lymphoma is located including adjacent lymph nodes before chemotherapy, The planned target volume (PTV) was forged with 1.5 cm margins given to the CTV. Daily fractions of 150, 180 and 200 cGy were used during RT. A dose of 1500 cGy was administered after CT, if full response is received from children less than 5 years of age, an average dose of 2000 cGy in the case of children less than 10 years of age with full response, and a dose of 2500 cGy in the case of those with partial response. Doses of 2500-3000 cGy were used in patients above 10 years of age with full response and doses of 3600-4140 cGy with boost in the case of those with partial response. Properties of RT area are given in Table 1. Briefly, mantle and mini mantle treatment portals account for half of the patients while IFRT was given in 30% of patients. IFRT encompasses a region, not an individual LN. Extended RT fields encompasses mini-mantle (bilateral cervical, SCF, infraclavicular, axilla), mantle (bilateral cervical, SCF, infraclavicular, mediastinal, hilar, axilla) and inverted Y (paraaortic, bilateral pelvic and inguino-femoral±splenic).
During follow-up of patients, complete response, partial response and progression were assessed. In addition, relapse treatment and outcomes were recorded. The data obtained was uploaded to SPSS 13.0 software. Kaplan- Meier test was used for survival time. Prognostic factors were calculated by long- rank test. Cox regression analysis was used for multivariate analysis. P<0.05 was considered significant.
A total of 44 patients, 29 of which (66%) were male, 15 of which (34%) were female, were included in the study. Mean age was 10.4 ± 4.2 (3-16). 69% of the patients were at the age of 10 years and above.
Their distribution by stage was as follows: 2 patient (5%) in stage 1A; 15 patients (34%) in stage 2A, 6 patient (13%) in stage 2B, 3 patient (7%) in stage 2S, 1 patients (2%) in stage 3A, 8 patients (19%) in stage 3B, 4 (9%) in stage 3S and 5 patients (11%) in stage IV (Stage I 5%, stage II 54%, stage III 30%, stage IV 11%). If the patients are rated by risk factors, 22 patients (50%) were in early stage favorable group, 4 patients (9%) were in early stage unfavorable group and 18 patients (41%) were in advanced stage.
According to the histological type, 9 patients (20%) were lymphocyte-predominant HL (LRHL), 15 (35%) were nodular sclerosing HL (NSHL) and 20 (45%) were mixed type HL (MCHL). At the time of diagnosis, 89% of the patients had an ECOG performance score of 0 and 1 and 32% had B symptom and 11% had Bulky disease. 7 patients (16%) had spleen involvement. Patient’s demographic characteristics and clinical data are shown in Table 2.
During follow-up, 4 patients (%9) relapsed (8-22 months). Patients who relapsed were given a 2. series of CT (COPP/OEPA), 1 patient received RT after CT, and the other 3 patients were monitored.
Median survival time was 164.32 ± 13.8 months in our patients with 168.4 ± 12.9 months for males and 106.8 ± 14.7 months for females. 1, 3, 5 and 10 year overall survival rates were 96%, 91.8%, 88.3% and %87.9, respectively (Table 3). According to risk groups, 1, 3, 5 and 10 year survival rates for early favorable group were 100%, 100%, 100% and 100% , respectively, early unfavorable group 98.8%, 93.5%, 88.1% and 80.2% respectively and for advanced stage 90.2%, 87.9%, 71.9% and 71.9%, respectively.
Several prognostic factors have been identified for Hodgkin's lymphoma. These are age, sex, B symptom, bulky disease, ECOG performance score and stage. In our study, age, sex, stage, histology, ECOG performance score, presence of symptom B and presence of bulky disease were evaluated. In univariate analysis, stage (p<0.005) and ECOG performance score (p<0.0001) were found to be variables with effects on overall survival. In multivariate analysis, only ECOG performance score (p<0.003) was found to be statistically significant. In Table 3, p values of prognostic factors are shown.
Pediatric Hodgkin’s lymphoma patients on follow-up in our clinic were studied retrospectively; efforts were placed on identifying their epidemiological and clinical features; success of the treatment applied and prognostic factors affecting survival were set forth.
Hodgkin’s lymphoma peaks twice with one around the age of 20, and the other around the age of 45 [1]. Its incidence before the age of 20 is high in developing countries, whereas it develops in later years in developed countries. Its incidence gradually increases after the age of 10 especially in developing countries depending on socio-economic reasons, and peaks at the age of 20 something. The problem is excessive industrialization in developed countries [5]. Although previous research reported a mean age at diagnosis of 7-8 years in Turkey, mean age at diagnosis of our patients was 10 [2,3,6].
In all age groups, it is more common in males. In our patients, male/female ration was 3/1. The most common types are mixed type and nodular sclerosing Hodgkin's lymphoma [5]. In our study, the most common type was mixed type for both sexes.
In Hodgkin's lymphoma, the disease usually occurs in peripheral lymph nodes (LAP) with painless growth at a rate of 90%. It is mostly seen in the cervical region. It has an elastic consistency and is painless. Also in the case of our patients, it developed with peripheral LAP at a rate of 92%.
Prevalence of B symptom varies in the range of 25 to 40% [7]. 31% of our patients had B symptom at the time of diagnosis.
In the literature, Hodgkin's lymphoma is most often seen in the early stages, and in our study, 58% of patients were in the early stage.
Standard treatment for early-stage Hodgkin's lymphoma involves CT (ABVD, MOPP, BEACOPP and Stanford V regimen) and IFRT. 44 of our patients received RT after CT (ABVD).
Possibility of developing secondary malignancy after treatment of Hodgkin’s lymphoma is on the increase. Leukemias may develop during the first five years, solid tumors with a majority of soft tissue sarcomas, thyroid, bone and breast cancers may emerge after 15 to 20 years [8,9]. No secondary tumor has been detected in our patients yet.
Previous studies reported the overall survival is 97% and the 3-year overall survival rates were 88% and 5-year overall survival rates were 88% [10,11]. Mean survival time and overall survival rates in our study were found to be comparable with literature.
There are many articles demonstrating that age, sex, B symptom, bulky disease, ECOG performance score and stage have prognostic importance in Hodgkin’s lymphoma [7]. Consistent with literature, stage and ECOG performance score in our study were statistically significant.
In conclusion, both epidemiological and post-treatment survival rates of our pediatric Hodgkin's lymphoma patients were consistent with the literature. However, further information about survival and incidence of secondary cancers can be obtained with increasing number of patients and time of follow-up.
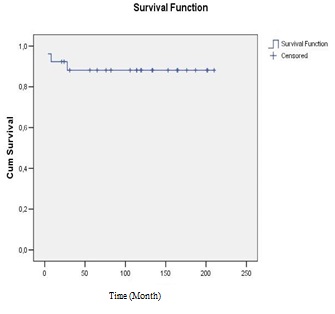 |
Figure 1: Overall survival |
n |
% |
|
|---|---|---|
IFRT |
13 |
30 |
Neck+SCF |
4 |
9 |
Mini- Mantle |
7 |
16 |
Mantle |
15 |
34 |
Mantle+İnverted Y |
5 |
11 |
| IFRT: involved-field radiotherapy, SCF:Supraclavicular fossa, Mini-mantle: Bilateral cervical, SCF, infraclavicular, axilla, Mantle: Bilateral cervical, SCF, infraclavicular, mediastinal, hilar, axilla, İnverted Y: Paraaortic, bilateral pelvic and inguino-femoral±splenic Table 1: Properties of RT Area |
||
n |
% |
|
Female/Male |
15/29 |
34/66 |
Age 10.4 ± 4.2 |
||
Histology |
||
LRHL |
9 |
20 |
NSHL |
15 |
35 |
MCHL |
20 |
45 |
B symptom |
14 |
32 |
Bulky |
5 |
11 |
Spleen involvement |
7 |
16 |
Stage |
||
I |
2 |
5 |
II |
24 |
54 |
III |
13 |
30 |
IV |
5 |
11 |
Early stage favorable |
22 |
50 |
Early stage unfavorable |
4 |
9 |
Advanced stage |
18 |
41 |
ECOG 0 |
27 |
62 |
ECOG 1 |
12 |
27 |
ECOG 2 |
4 |
9 |
ECOG 3 |
1 |
2 |
Latest status |
||
Alive/Dead |
39/5 |
89/11 |
LRHL: Lymphocyte-predominant HL, NSHL: Nodular sclerosing HL, MCHL: Mixed type HL |
||
| Variable | p |
|
|---|---|---|
Univariate |
Multivariate |
|
Age |
0.235 |
|
Sex |
0.698 |
|
Stage |
0.005 |
|
Risk factors |
0.108 |
|
Histology |
0.546 |
|
ECOG status |
0.0001 |
0.003 |
B symptom |
0.006 |
|
Bulky |
0.342 |
|
Relapse |
0.511 |
|
Table 3: Prognostic Factors |
||






































