Top Links
Journal of Dentistry and Oral Care Medicine
ISSN: 2454-3276
In Vitro Comparison of Margin Fracture Strength of E.MaxTM and EmpressTM Inlays
Copyright: © 2015 Maseli V. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Related article at Pubmed, Google Scholar
Ceramic restorations are appealing because of their esthetics, high hardness and wear resistance. They can replace a composite or amalgam restoration in teeth where buccal and lingual walls remain intact and where excessive isthmus width contraindicates the use of a direct posterior composite restoration. Recent clinical trials have shown that porcelain restorations with margins on the occlusal surface of a posterior tooth tend to fail due to fracture of the porcelain under biting forces. Small chips initiate stress patterns that can lead to bulk material fracture overtime as the restoration is in function. Previous in vitro studies have tested the fracture resistance by using load perpendicular to the central groove of the inlay restoration. The purpose of this study is to compare the margin fracture strength of MOD inlay restorations with two different occlusal angles and fabricated with IPS EmpressTM and IPS e.maxTM ceramic inlay restorations. Four groups of 10 samples each were tested: A: 45º/e.maxTM, B: 45º/EmpressTM, C: 60º/e.maxTM and D: 60º/EmpressTM. A rod with a 1mm diameter radius, mounted in an Instron testing machine was used to apply compressive loads on the occlusal margins within 1mm of the interface at a crosshead speed of 0.5mm/min until fracture. Mean load values were: A: 592.1 MPa, B: 455.3 MPa, C: 494.5 MPa and D: 274.8 MPa. For both e.maxTM and EmpressTM, the 45º angled margins were significantly stronger than the 60º margins. For both margin angles, e.maxTM porcelain had significantly stronger margins than EmpressTM. The thicker margins (45º angles) were stronger than the thinner margins (60º angles) for both e.maxTM and EmpressTM.
The occlusal anatomy, margin design and porcelain material are critical factors that significantly affect the margin strength of inlay/onlay ceramic restorations.
Keywords: Dental porcelain; Partial coverage restorations; e.maxTM; EmpressTM; Fracture resistance; Compressive strength
Ceramic restorations are appealing because of their esthetics, low density, high hardness, wear resistance and high survival rate [1-4]. Ceramic inlays can be conservative of tooth structure [5]. They can replace a metal-casting or amalgam restoration in patients who require a class II restoration where buccal and lingual walls remain intact, and offer a viable alternative where excessive isthmus width contraindicates the use of a direct posterior composite restoration [6]. Their brittle nature though can be a limitation [7,8].
The margins of any type of restoration are important not only for the survival of the restoration itself but also for the periodontal health of the soft tissues and for reducing susceptibility to recurrent decay. Smooth and even margins are essential [9-14] and a fit of 50-100μm is desirable to avoid excessive exposure of cement [15]. Marginal adaptation is defined as the accuracy of fit between a restoration and tooth at the cavosurface [16]. Accurate fit of a restoration is related to both laboratory and clinical technique [16]. Poor marginal adaptation results in retention sites for microorganisms that can migrate to the bottom of the cavity preparation and release toxins/products that can damage the pulp [17,18]. The use of dual-cure resin cement is recommended for better margin support and enhanced durability [19-25].
Recent clinical trials [26,27] have shown that porcelain restorations with margins on the occlusal surface of a posterior tooth tend to fail due to fracture of the porcelain under biting forces. Small chips initiate stress patterns that can lead to bulk material fracture over time as the restoration is in function. This has been seen in two, three-year clinical projects that have been reported at major research meetings [26,27]. Laboratory projects have also been conducted to assess the relationship of the cavity preparation design to the area of initial crack formation and to the strength of the porcelain restoration under simulated stress to maximum loading. These studies have shown the porcelain to be reasonably strong in the center of the restoration when the thickness is at least 2 mm [4,13,28-31]. A ''c'' shape or mosaic fracture pattern has been noticed over time [12,14,32,33]. However, some investigators stated that reduced thickness of ceramic is not a limitation [12,14,32,34,35]. Failure analysis of clinical cases shows that the failure occurs most frequently at the junction of the porcelain and the tooth (the margin). Edge strength can be described as the ability of restorative materials to withstand fracture at 0.5 mm of a thin edge [36-42]. The force-to-fracture increases significantly as the distance from the edge increases [36,39,41].
Dental porcelain materials can be classified based on the microstructure of a ceramic and on processing technique [43].
Microstructure includes: 1) glass-based systems (mainly silica), 2) glass-based systems with fillers, usually crystalline (feldspathic, leucite reinforced and lithium disilicate), 3) crystalline-based systems with glass fillers (mainly alumina) and 4) polycrystalline solids (alumina and zirconia).
Processing includes: 1) powder/liquid, 2) pressable, 3) CAD/CAM and 4) glass-infiltrated. The flexural strength of lithium disilicate is approximately 360MPa or about three times that of EmpressTM (160 MPa) [43-47].
Previous studies have tested the fracture resistance by using load perpendicular to the central groove of the inlay restoration where the material is thicker than near the margin [14,23-25]. It may be significantly different when the load is applied to the buccal and lingual inclinations at a position near the margin interface.
The purpose of this study was to compare the margin fracture strength of MOD inlay restorations with two different occlusal margin angles fabricated with IPS EmpressTM or IPS e.maxTM porcelain. The null hypotheses were: (1) there is no difference in occlusal margin fracture strength of inlay restorations between the two different porcelain angles, (2) there is no difference in occlusal margin fracture strength between IPS EmpressTM and IPS e.maxTM ceramic restorations and (3) the model system developed for this study is a reliable test to evaluate porcelain margin fracture resistance.
For this in vitro study, a master die with a mesial-occlusal-distal preparation was fabricated in brass (Figure 1). A corresponding stainless steel guide with a 45º and 60º angled surface was also fabricated (Figure 2). The master preparation die was duplicated with a resin (Viade Products, Camarillo, CA, USA) which has a modulus of elasticity (12.9 GPa) similar to tooth dentin. The dimensions of the MOD cavity were: box depth: 4 mm, pulpal floor depth: 2 mm, axial wall height: 2 mm and isthmus width: 5 mm [6]. Figure 3 is a cross-sectional view of the two wax patterns formed with the 45º and 60º inclination. The restoration fabricated with the 60º inclination will have steeper anatomy and be thinner at the occlusal margin than the 45º inclination, which will have shallower anatomy and be thicker at the margin. A total of 40 specimens (sample size determined by previous studies [36-41] were tested.
Die spacer (Taub Rubber Sep, pink, #10-2002, TAUB Products, Jersey City, NJ) was applied to the pulpal floor, axial and cervical walls in a thin layer to within 1 mm from the margins. Wax patterns were made on the resin dies. To form the wax on the occlusal surface to 45º and 60º, angles, the stainless steel guide was heated and passed over the wax pattern to produce the desired margin. The wax patterns were sent to a dental laboratory to press the corresponding ceramic monolithic inlays. The dies were selected at random and the wax patterns, dies and ceramic inlays were coded, so that each inlay was placed on the resin die from which the pattern was fabricated. The glazed inlays were seated in the dies and the fit was checked using an explorer under magnifying loopes 2.5x (Orascoptic, Middleton, WI). A resin cement (Nexus Third Generation, NX3 dual-cure, Kerr, Orange, CA) was used according to the manufacturer's instructions to cement all the inlays. The internal surface of the porcelain was etched with Ultra-etch (9.6% buffered Hydrofluoric Acid, Ultradent Products, Inc., S. South Jordan, UT) for 1 minute and silane primer was applied (Kerr, Orange, CA) for 1 minute and lightly air-dried. The die was etched with 37% hydrophosphoric acid for 15 seconds, rinsed and air-dried. Optibond Solo (Kerr,Orange, CA) was applied with a microbrush, air-dried for 3 seconds and light-cured for 10 seconds. Nexus 3 was dispensed to the internal surface of the inlay restoration, seated in the die with finger pressure and excess cement was removed with a microbrush. The restoration was placed under a load of 10 gr, and each surface was light cured for 20 seconds. The load was removed from the die and the occlusal surface was light cured for 40 seconds (Figure 4). All light curing was performed using the VALO curing light (Ultradent Products, Inc. S. South Jordan, UT) at a light intensity of 950 mW/cm2. Light efficacy/power was tested every 10 samples with a visible curing light meter (Cure Rite, Dentsply, Milford, DE). Excess cement was removed with a No 15 Bard Parker blade (Aspen SurgicalTM Caledonia, MI) but no finishing was done on the margins. A sharpie marker (Sharpie®, Downers Grove, IL) was used to indicate the point of loading 1 mm away from the occlusal margin. Two diametrically opposite margin points were marked on each sample and the specimens were stored in a dark humidor for 48 hours before testing. A stainless steel probe with 1 mm diameter (area = 0.7854 mm2) was mounted in an Instron universal testing machine (Instron 5565, Instron Industrial Products, Grove City, PA and software Bluehill 3) and used to apply compressive loads within 1 mm of the interface at a 0.5 mm/min crosshead speed until initial crack formation was visible. The load was applied perpendicular to the inclined surface by holding the die in a custom jig adjusted in a protractor (Figure 5). The load at initial crack formation was determined by the Instron software. Two values were obtained (one at each marked point) and a mean value was derived for each restoration. After loading and margin fracture, 2 dies were selected from each group, one with the highest margin fracture strength and one with the lowest. The selected dies were trimmed and embedded in clear orthodontic acrylic (KoldMount, Nobilium Company, Albany, NY) for sectioning. The embedded dies were sectioned buccal-lingually at the point where the load was applied using a diamond wheel saw (Model 650 Low Speed Diamond Wheel Saw, South Bay Technology Inc., San Clemente, CA). Qualitative fracture pattern evaluation was performed under a microscope (Nikon SMZ1500, Nikon Instruments, Inc., Melville, New York) at 10X magnification with high intensity illumination and photos were taken using the Image ProPlus software and SPOT Advanced camera (SPOT Imaging Solutions, a division of Diagnostic Instruments, Inc. Sterling Heights, Michigan). Means and standard deviations were calculated for each group and statistically analyzed using 2-way ANOVA and an independent t-test, with significance at p<0.05 (XLSTAT software, Statistical Innovations, Belmont, MA).
To confirm that the ceramic inlay restorations were properly seated in the dies, 4 samples (one sample for each group) were fabricated following the same procedures. The inlays were tried-in and the fit was checked using an explorer across the occlusal and cervical margins to document clinical integrity. Super glue was used at the cervical margins to stabilize the restoration in place. The samples were embedded and sectioned buccal-lingual in the center of the restoration.
The purpose of this study was to compare the margin fracture strength of MOD inlay restorations with two different occlusal angles fabricated with IPS EmpressTM and IPS e.maxTM porcelain.
The margin fracture strength of 40 restorations was measured, ten samples in each group. Mean load values were: 592.1 MPa (e.maxTM/45º), 455.3 MPa (EmpressTM/45º), 494.5 MPa (e.maxTM/60º) and 274.8 MPa (EmpressTM/60º) (Table 1).
A statistically significant difference was found between the 2 materials and the 2 occlusal angled surfaces and Ho1 and Ho2 were rejected. IPS e.maxTM/45º inlays and IPS EmpressTM/45º were significantly stronger than IPS e.maxTM/60º and IPS EmpressTM/60º respectively. In addition, e.maxTM/60º was significantly stronger than EmpressTM/60º and e.maxTM/45º was stronger than EmpressTM/45º.
The highest margin strength value was noticed in the e.maxTM 45º group (#6 sample; a: 682.5 MPA, b: 762.7 MPA) and the lowest margin strength in the EmpressTM 60º group (#9; a: 129.9 MPa b: 255.9 MPa).
The 2-way ANOVA (Table 2) showed that the material and the angle were both significantly different with no interaction. The Ho3 was accepted, since the model system developed for this study was effective at determining significant material and angle differences.
The following pictures (Figures 6 and 7) show the occlusal surfaces of ceramic restorations after loading. A mode of fracture was observed for all 4 groups. The initial crack had a ''c'' shaped pattern along the margin. For the e.maxTM 45º inlays, the initial fracture was limited to the loading area and did not extend into the occlusal surface (Figure 6): whereas the other groups tended to propagate more quickly into a bulk fracture (Figure 7). In general, the 45º groups had less severe fracture on the occlusal surfaces than the 60º groups.
The qualitative internal fracture pattern evaluation of the sectioned samples showed that there was not a consistent internal fracture pattern. The only common characteristic in these cross-sectional views was that the fracture point started at the loading point and propagated into the bulk of the ceramic restoration. The fracture pattern observed was either fixed (crack is one direction) (Figure 8) or multidirectional (several cracks in different directions) (Figure 9). There was no correlation between the internal fracture pattern and margin fracture strength. This behavior was evident for both the EmpressTM and e.maxTM materials and for both 45º and 60º occlusal angles.
This in vitro study compared and evaluated the margin fracture strength of two different porcelain MOD inlay restorations with two different occlusal angles. In this study, pressable leucite reinforced ceramic (EmpressTM) and pressable lithium disilicate ceramic (e.maxTM) were compared. The rationale for 2 different occlusal surfaces (45º -thicker margin and 60º -thinner margin) was that clinically the final ceramic thickness may be less if occlusal anatomy is steeper and after occlusal adjustment [28]. It was anticipated that the risk for fracture may be higher in the case of a 60º angle of the porcelain at the margin area.
Other investigators have performed the evaluation of ceramic fracture strength by applying the load vertical to the center of the restoration (occlusal central fissure of inlay restoration) [19,28,44]. In these studies, ceramic restorations were extended to the functional cusp and were cemented to extracted teeth [28]. Using Finite Element Analysis (FEA) models [19,34,35], variables such as width of preparation and volume of ceramic were evaluated. Bar-shaped [38] specimens and disk samples have been used to determine the edge strength of porcelain in which force was applied 0.5-1.0 mm from the edge of the sample (edge strength) [36,37,39,41]. In this in vitro study, samples had an actual inlay restoration shape and load was applied perpendicular to the buccal and lingual inclines of the restoration. One preparation design was used for preparation consistency and to decrease variables. The indenter was placed 1 mm away from the margin to avoid the load being placed on the die-restoration interface. This is the reason why the test is called margin fracture strength and not edge strength.
The mean margin fracture strength of e.maxTM (lithium disilicate) ceramic material was significantly higher than that of the EmpressTM (leucite reinforced) ceramic, which is in agreement with other studies [44-47]. This increased fracture strength can be attributed to the increased percentage of crystallinity (up to 70%) of this porcelain material as well as a more refined crystal size [43,46]. There was a significant difference in the fracture strength between the two ceramic materials and between the two occlusal angles, indicating that the test design and method were satisfactory to identify significant differences.
It is difficult to standardize the preparation design for ceramic inlays clinically because of the uniqueness and complexity of each clinical situation. In the literature, there has been a consensus to have 1.5-2.0 mm as ideal thickness for ceramic restorations [6,13,28-31]. The width of the inlay preparation should not exceed 1/3 of the total width of the tooth because the increased inlay width reduces tooth structure and increases the stress on the restoration [19]. The die for this study was constructed within these guidelines, but the restoration fabricated with the 60º inclination was thinner at the occlusal margins (steeper anatomy) than the 45º inclination (shallower anatomy), as seen in Figure 3.
However, Holberg [34,35] reported that a reduced thickness (0.7 mm) of lithium disilicate inlays did not increase the fracture risk of the restoration. Kramer also found no correlation between ceramic thickness and ceramic fractures [12,14,32]. The properties of the material were more important (EmpressTM vs e.maxTM). Several authors suggested 1.5 mm of minimum ceramic thickness for EmpressTM inlays because of higher risk of fracture during the cementation procedure [12,14,32].
The cementation was performed with dual-cure resin cement (Nexus Third Generation, NX3 dual-cure, Kerr, Orange, CA), as preferred for posterior ceramic cementation in other studies [20-22,28]. A total etch resin cement (Variolink II) performed better in the occlusal margin adaptation than a self-adhesive cement (Rely X Unicem) because the increased amount of water sorption of self-adhesive resin leads to a higher amount of wear at the occlusal enamel margins of the restoration [20-22,28]. According to Isidor, et al. [23], leucite reinforced ceramic inlays had more failures with light-cure cement than dual-cure cement. Beier, et al. [24], recommended a high viscosity dual-cure cement, while Stoll, et al. showed that there was no difference between low and high viscosity dual-cure cements [25]. On the contrary, Federlin, et al. [28], reported that there was no difference in crack formation between dual-cure and self-adhesive cement and crack formation was influenced by ceramic thickness. Finally, a marginal fit of 50-100 μm was recommended to avoid excessive marginal wear [22]. The die used in this study had a modulus of elasticity similar to dentin and was prepared by micro-abrasion and acid washing to simulate the roughness of etched tooth structure. The cement was used to enhance retention and reinforce the porcelain during the test.
Occlusal margins were checked clinically with an explorer for seating and a 10g load was applied on the occlusal surface of the restoration after cement placement. However, in the magnified cross-section pictures, occlusal margins were overextended and were lacking ideal adaptation (Figures 8, 9 and 10). The overextended occlusal margins could be attributed to the thickness of die spacer or a discrepancy in occlusal margin adaptation between wax pattern and ceramic restoration. Variations in the laboratory procedures were controlled to some extent by using one experienced technician [9]. Ceramic defects can also occur in occlusal margins and a perfect adaptation of the ceramic to the tooth is influenced by the irregular cavity outline [9].
At the microscopic magnification, it was observed that occlusal margins appeared slightly overextended and marginal adaptation was compromised. The fit of the uncemented inlays was similar to that seen in the cemented samples (Figure 10). Occlusal margins were overextended and the adaptation of ceramic restorations at the pulpal floor of the prepared die was not ideal.
A specific mode of fracture was observed in the occlusal surface of all restorations. The crack initiation had a ''c'' shape translucent pattern along the margin which progressed in some cases to a ''line'' formed along the proximal marginal ridges. ''Half-moon'' fractures also were detected in the studies of Kramer and Frankenberger [12,14,32]. This fracture pattern was limited to the area where the load was applied. Hayashi, et al. [33] also noticed cracking or chipping in a mosaic pattern of the ceramic.
There was not a consistent internal fracture pattern in the cross-sectional views of the tested samples. The only common characteristic was that the fracture line had a start point on the load area and propagated into the bulk of the ceramic restoration. The fracture pattern observed was either multidirectional (several cracks in different directions) or fixed (crack is in a single direction). There was no correlation between fracture pattern and margin fracture strength. This behavior was evident for both the EmpressTM and e.maxTM materials and is consistent for brittle materials like ceramics. It was also seen that the first loading on a side of each sample did not affect the margin fracture strength of the b side. There were samples that presented higher margin fracture strength values in b side that a side (Figure 6 and 7).
This study showed that the marginal design should be decided carefully and accurately to avoid excessive loading on a thin margin. Previous studies have recommended that occlusal contact close to the ceramic/tooth interface should be avoided because of the high risk of debonding and fracture [19,41] and that occlusal force leads to marginal deterioration and growth of microcracks [15]. As a result, shallower occlusal anatomy will develop thicker and more fracture resistant occlusal margins.
To avoid overloading a thin margin, a ceramic inlay restoration should not be considered as a treatment option in cases of unfavorable occlusion or parafunctional activity (bruxism) [6]. In a clinical study, Beier, et al. [4] did not find greater risk of failure associated with existing bruxism but the occlusal scheme provided was canine guidance, eliminating all balancing contacts. An occlusal bite splint was also provided to the patients to minimize stress concentration. In patients who had severe bruxism, cast gold restorations might be the treatment of choice.
Future studies could include the development of materials with improved properties such as ceramics with a modulus of elasticity close to that of dentin or a more elastic luting agent for stress relief and to provide marginal stability over time. This study design was adequate to show a significant difference between margin angles and porcelain materials, so it could be extended to compare a variety of other porcelain materials. Loading could be applied using a different shape and size of indenter, different load directions or using cyclic loading patterns. It is also important to further evaluate the cement space and the die spacer material in order to improve internal fit and occlusal margin adaptability.
• The e.maxTM (lithium disilicate) ceramic inlays had significantly higher margin fracture strength than EmpressTM (leucite reinforced) at both 45º and 60º margin angles.
• The 45º inlays were significantly stronger than the 60º inlays for both e.maxTM and IPS EmpressTM.
• The margin strength test was effective at determining significant material and angle differences.
The occlusal anatomy, margin design and porcelain material are critical factors that significantly affect the margin strength of inlay/onlay ceramic restorations.
This work was partially supported by the Delta Dental Foundation.
 |
| Figure 1: Brass master die, A. proximal view, B. occlusal viewMaterials |
 |
| Figure 2: Stainless steel form with a 45o and 60o angled surface; A. top view, B. profile view |
 |
| Figure 3: Wax pattern design, cross-section view with occlusal margin angles noted |
 |
| Figure 4: Cemented restorations with 45º (A) and 60º (B); proximal views showing occlusal margin profile |
 |
| Figure 5: Instron Univeral Testing Machine (Instron 5565)/Protractor, Custom jig |
 |
| Figure 6: e.maxTM inlay (45º angle) with the highest value a: 682.5 MPa, b: 762.7 MPa) showing a ''c'' shape fracture pattern |
 |
| Figure 7: EmpressTM inlay (60º angle) with the lowest value (a: 129.9 MPa, b: 255.9 MPa) showing immediate bulk fracture pattern |
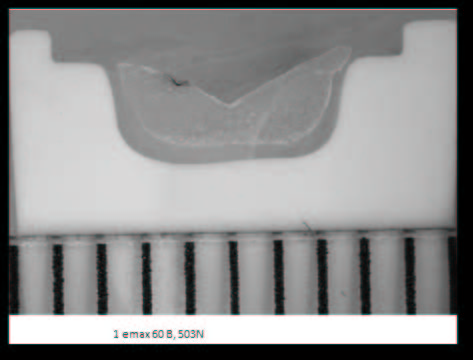 |
| Figure 8: Cross-section view of cemented inlay (e.maxTM 60º) after fracture. Divisions below model represent 1 mm increments |
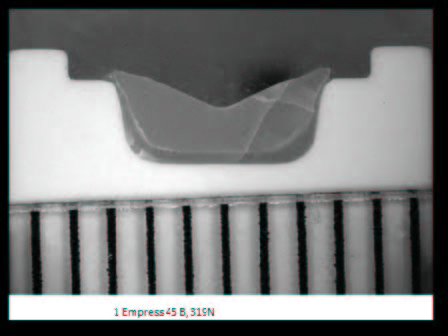 |
| Figure 9: Cross-section view of cemented inlay (EmpressTM 45º) after fracture. Divisions below model represent 1 mm increments |
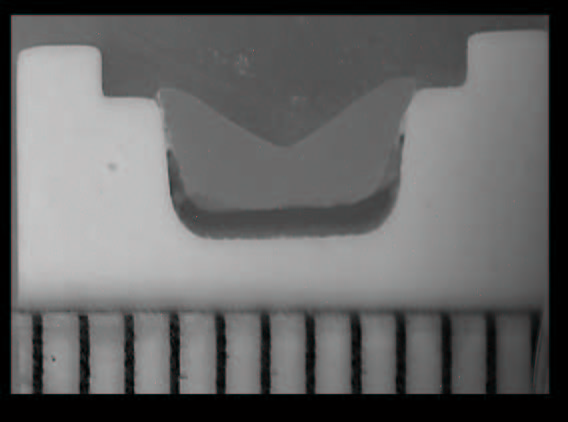 |
| Figure 10 Cross-section view of non-cemented and non-loaded inlay (e.maxTM 45º). Divisions below model represent 1 mm increments |
| 60o | 45o | P | |
|---|---|---|---|
| IPS e.maxTM | 494.46 (80.5)a | 592.06(103.2)a | 0.03 |
| IPS EmpressTM | 274.76 (49.9)a | 455.31(67.4)a | <0.01 |
| p | <0.01 | <0.01 | |
| a: statistically significant difference (p<0.05) using independent t-tests Table 1: Mean values (SD) of margin fracture strength (MPa) |
|||
| Source | Sum of Squares | Degrees of Freedom | Mean Square | F-Ratio | P-Value |
|---|---|---|---|---|---|
| Material | 195930.006 | 1 | 195930.006 | 52.598 | 52.598 |
| Angle | 119301.006 | 1 | 9301.006 | 32.027 | 0.000a |
| Material*Angle | 10611.306 | 1 | 10611.306 | 2.849 | 0.100b |
| Error | 134101.025 | 36 | 3725.028 | ||
| a: statistically significant difference (p<0.05), b: no interaction (p>0.05) Table 2: 2-way Analysis of Variance |
|||||






































