Top Links
Journal of Case Reports and Studies
ISSN: 2348-9820
Contralateral Delayed Acute Subdural Hematoma Following Evacuation of a Chronic Subdural Hematoma with Burr-Hole Craniotomy and Continuous Closed System Drainage: Case Report and Literature Review
Copyright: © 2016 Rong-Dar Tzou. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Related article at Pubmed, Google Scholar
Chronic subdural hematoma (CSDH) is a relatively frequent problem in neurologic or neurosurgical practice. Treatments for CSDH are well established and provide positive postoperative outcome; however, some atypical postoperative complications can occur. This study reports a rare complication of delayed contralateral acute hematoma following the evacuation of a chronic subdural hematoma with burr-hole craniotomy and continuous closed system drainage. According to our research, our study is the first to report a delayed contralateral acute subdural hematoma following CSDH surgery.
Keywords: Delayed contralateral acute subdural hematoma; Chronic subdural hematoma; Burr-hole craniotomy; Closed system drainage; Complication
List of Abbreviations: CSDH: Chronic subdural hematoma; CASDH: Contralateral acute subdural hematoma; CT: Computed tomography
Chronic subdural hematoma (CSDH) is a relatively frequent problem in neurologic or neurosurgical practice [1]. The potential for recovery from the evacuation of a CSDH is relatively high. However, some postoperative complications may affect the postoperative course [2]. In this study, we report a rare complication of contralateral acute hematoma following the evacuation of a CSDH with burr-hole craniotomy and continuous closed system drainage.
A 78-year-old man presented with weakness in his right-side extremities and gait disturbance. He had a medical history of chronic kidney disease, dementia, and hypertension. Upon admission, a neurological examination revealed right hemiparesis (muscle power, 4 of 5), poor orientation in person and place, and isocoria with normal light reaction. The results from hematological investigations, biochemistry tests, and coagulation profile were within normal ranges. Computed tomography (CT) of the head showed a hypodense subdural hematoma over the left frontoparietotemporal region, causing a midline shift to the right and compression of the ipsilateral lateral ventricle (Figure 1A). A left chronic subdural hematoma was diagnosed. Burr-hole evacuation of the hematoma with continuous closed system drainage was performed immediately.
On Day 5, CT of the head was performed and near complete evacuation of the hematoma was observed (Figure 1B). However, on Day 6, the patient had an altered level of consciousness following the sudden efflux of a large amount of subdural effusion from the drainage system. CT of the head revealed an acute subdural hematoma on the contralateral side, with a midline shift to the left and compression of the ipsilateral lateral ventricle (Figure 1C). Under general anesthesia, a craniotomy was made over the right frontotemporoparietal region, and the subdural hematoma was observed in the space between the dura and an inner membrane (Figure 2A). Following the removal of the hematoma, bleeding from the torn bridge vein was observed, and the bleeding vein was coagulated (Figure 2B). An intracranial pressure monitoring system provided measurements of intracranial pressure at a subdural level, and consistently low intracranial pressure (-3-5mmHg) was recorded. The second postoperative course was uneventful. The patient was discharged 20 days later with mild neurological deficit.
A contralateral hematoma is a rare complication following the evacuation of a CSDH and has been well described previously (Table 1). The contralateral hematoma commonly occurs immediately. Rarely, the contralateral hematoma develops 6 days postsurgery. In this study, we report an unusual case of delayed contralateral acute subdural hematoma (CASDH) following the evacuation of a CSDH.
The pathophysiological mechanisms underlying a contralateral acute intracranial hematoma following burr-hole craniotomy with continuous closed system drainage are unclear. Several possible mechanisms could be responsible for contralateral acute hematoma development. The abrupt evacuation of a CSDH might result in a brain parenchyma shift, leading to contralateral bridge vein or cortical vein disruption [3-5]. Alternatively, a decrease in the intracranial pressure after the evacuation of a hematoma might disturb vascular autoregulation in patients suffering from chronic elevated intracranial pressure [3-7].
Hemorrhage into previously undetected areas of a contusion could also be responsible [3,4]. The rapid evacuation of a hematoma, disturbance of autoregulation, and presence of an undetected lesion are other possible causes. However, in our reported case, these mechanisms would not explain the presence of a delayed contralateral acute hematoma. Chronic intracranial hypotension is a risk factor for delayed acute hematoma. In conditions of intracranial hypotension, the brain cannot be fully supported, and the tensed bridge vein can easily damage.
Whether a contralateral acute hematoma can be avoided remains unclear. Minimal evidence exists to support the use of perioperative or postoperative methods in patients with chonic subdural hematoma undergoing burr-hole craniotomy and continuous system drainage. Modesti et al. [4] suggested using decompression with a slow rate of evacuation during the perioperative period to avoid an abrupt brain parenchyma shift. Kiymaz et al. [8] indicated that continuous drainage therapy for CSDH provides superior results to one-time drainage methods. However, intermittant drainage might provide an alterative procedure to continuous drainage to avoid the rapid evacuation of a hematoma postsurgery. An appropriate fluid supplement should be administered to avoid chronic intracranial hypotension.
According to our research, our study is the first to report a delayed CASDH following burr-hole craniotomy with continuous closed system drainage. Our results indicate that the slow decompression of a CSDH and careful regulation of intracranial hypotension could prevent a delayed contralateral acute hematoma.
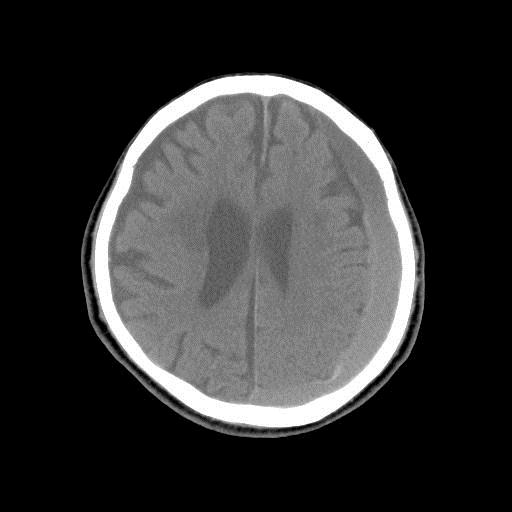 |
| Figure 1A: Preoperative CT revealing a hypodense subdural hematoma over the left frontoparietotemporal region, causing a midline shift to the right and compression of the ipsilateral lateral ventricle |
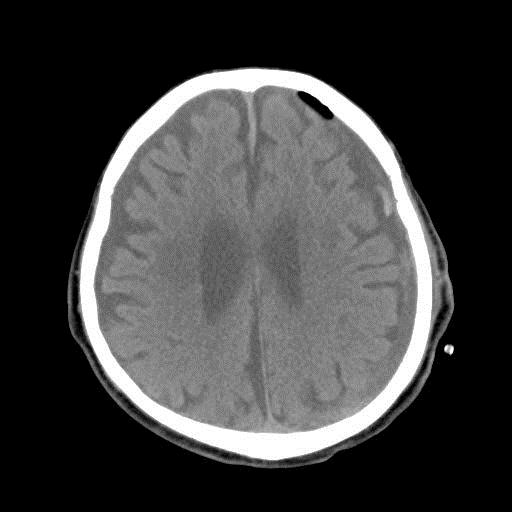 |
| Figure 1B: First postoperative CT showing near complete evacuation of a left CSDH |
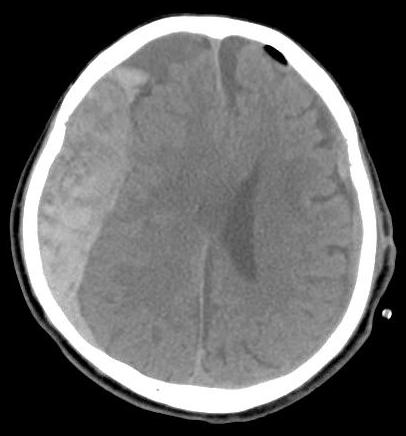 |
| Figure 1C: Postoperative CT revealing a contralateral acute hematoma, suggesting a subdural hematoma with a midline shift to the left and compression of the ipsilateral lateral ventricle |
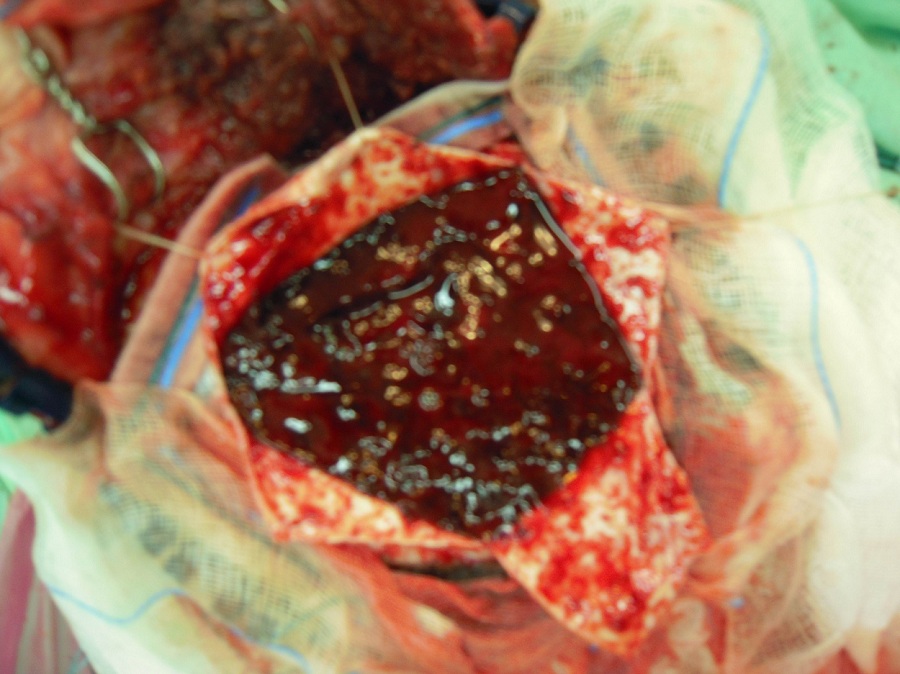 |
| Figure 2A: Intraoperative photograph, showing the hematoma beneath the dura matter |
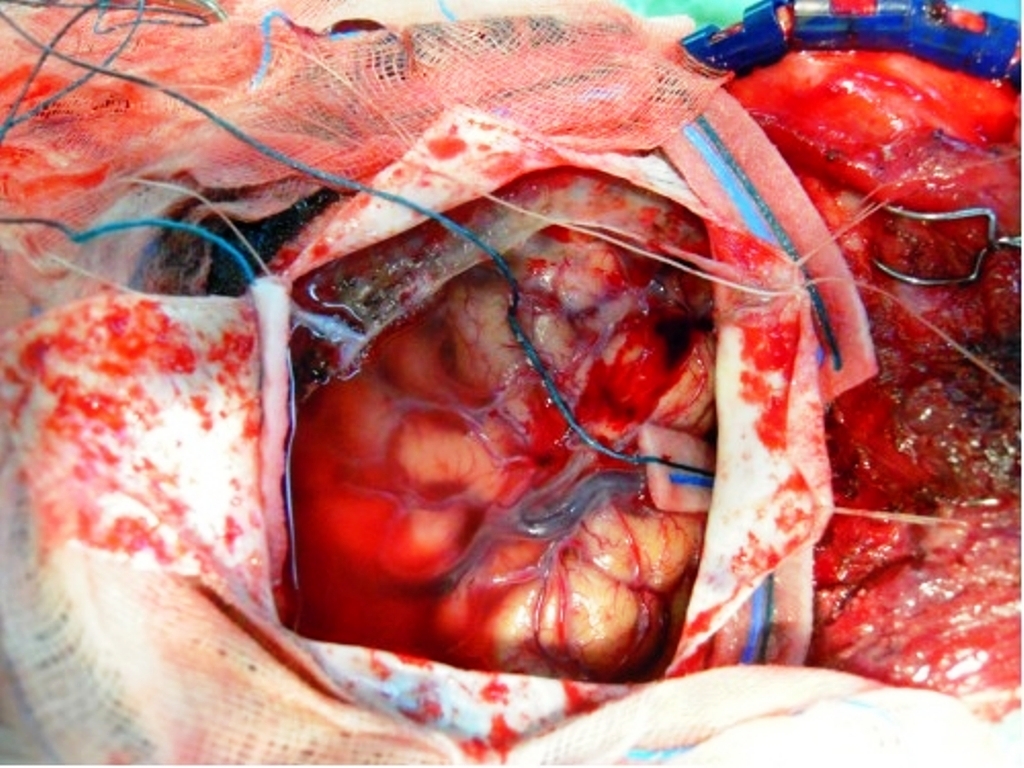 |
| Figure 2B: The partial removal of an inner membrane below the hematoma |
Author/ year |
Age/Gender |
Type of hematoma |
Mechanism |
|---|---|---|---|
Eom KS et al. [2] (2009) |
78/M |
AIDH |
The formation of a contralateral hematoma remains unclear. |
Panourias IG et al. [9] (2006) |
86/F |
AEDH |
The rapid evacuation of the chronic subdural hematoma decreased the high intracranial pressure and caused shift of the brain to the affected side. |
Liang CL et al. [10] (2001) |
44/M |
ASDH |
Rapid brain shifting may have torn the contralateral draining vein |
Su TM et al. [3] (2001) |
78/F |
ASDH |
Bleeding from a torn bridging vein secondary to perioperative parenchyma shift |
Turgut M et al. [1] (1998) |
66/M |
ASDH |
Brain compression and shift may tear also “contralateral” draining veins. Sudden increase in cerebral blood pressure combined with focal disruption of autoregulation. |
Harada K et al. [11] (1992) |
71/M |
ASDH |
The membranous layer separation then damaged the bridging vein and superior sagittal sinus |
Nagata K et al. [12] (1986) |
59/M |
ASDH |
Coagulopathy and the acute decrease of intracranial pressure. |
Our case |
78/M |
Delayed ASDH |
A long standing intracranial hypotension is a risk factor for delayed acute hematoma |
AIDH: Acute Interdural Hematoma; AEDH: Acute Epidural Hematoma; ASDH: Acute Subdural Hematoma |
|||






































