Top Links
Journal of Case Reports and Studies
ISSN: 2348-9820
A Rare Case Report of a Child Coexistence Thyroglossal Cyst and Second Branchial Cleft Fistulae
Copyright: © 2016 Mahdoufi R. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Related article at Pubmed, Google Scholar
Congenitalcervical anomalies are important to consider in the differential of head and neck masses in children and adults. These lesions can present as palpable cystic masses, infected masses, draining sinuses, or fistulae. Thyroglossal duct cysts are most common, followed by branchial cleft anomalies. A synchronous presentation of both type of cyst and fistula in a same child patient is very rare with no such cases reported in literature till date.
Keywords: Branchial fistula; Thyroglossal cyst; Coexistence; Child
Thyroglossal duct cysts account for approximately 70% of all congenital abnormalities of the neck. Anomalies of the second branchial fistula account for 90% of the developmental abnormalities of the branchial apparatus. But a simultaneous presentation of second branchial cleft fistulae with thyroglossal cyst is a very rare presentation. We present the first case of thyroglossal duct cyst and left branchial sinus which appeared concurrently in a same patient and which is very rare finding not reported in the literature.
An 8 year-old girl was admitted to our ENT department for recurrent, pain with lateral cervical discharge from a fistula in the lower part of the neck since birth. She also complained of a smooth lump on middle upper part of the neck for six month duration which increased in size with time.
On physical examination, there was a discharging defect along the left anterior border of Sternocleidomastoid muscle (SCM) at the junction of middle and upper 1/3rd of neck, an anterior palpable cervical mass at the level of the hyoid bone and it moves on swallowing and protrusion of the tongue. However no active inflammation was present around the lesions. Oropharynx and neck palpation were normal with no loco regional lymphadenopathy. Also there was no sign of other congenital anomalies inhead neck region or elsewhere.
According to the above findings, our clinical diagnosis is thyroglossal cyst and chronic skin sinus left upper neck. Ultrasound neck showedcystic lesion at the midline region of the neck likely of thyroglossal cyst. Sinus opening has medium tract which ends within the carotid bifurcation.
After necessary routine investigations, excision of the fistulous tract and thyroglossal cyst were carried out under generalanesthesia.
During the operation, the thyroglossal cyst was removed completely together with part of the hyoid bone as a standard Sistrunk operation. Excision of fistulous tract was done through elliptical one incision. Whole tract was removed, the upper blind end which blends with carotid bifurcation (Figure 1). Post-operative period was uneventful and patient was discharged one day after.
Histology of both specimens confirmed the diagnosis of thyroglossal duct cyst (Figure 2) and branchial fistulae (Figure 3).
No recurrence of symptoms is seenwith 6 months of follow-up.
Thyroglossal duct cysts (TGDCs) followed by branchial cleft anomalies are the most common congenital neck masses encountered in practice, Second branchial cleft cysts and sinuses are the most common type [1]. Although both abnormalities are common individually, but rarely seen associated in same patient as described in our case.
TGDCs are the most common congenital midline neck masses that arise from a tubal remnant of thyroid descent during development; it can be located anywhere along the course of the thyroglossal duct from the base of the tongue to the thyroid gland [2,3].
Patients present commonly with an asymptomatic, cystic neck mass in themidline near the hyoid bone, 66% of the location for thecystic mass is adjacent to the hyoid bone [3,4]. About 75% of patients with TGD anomalies are diagnosed before 30 years of age, and more than half of these are identified before age 10years [2], same thing reported in this case.
Clinically, the presentation of our case was classic, whether TGDCs move upward on tongue protrusion and swallowing [5,6]. However, restricted movement of the cyst does not rule out diagnosis. TGDCs may show similarities to dermoid cysts, lymphadenopathy, lymphatic malformations, ectopic thyroid gland, branchial cleft cysts, hemangiomas, lipomas, and sebaceous cysts [6,7]. Thyroglossalduct carcinomas occur in less than 1% of TGDCs [8,9].
Ultrasonic Image (USI) is considered the method of choice for confirming clinical diagnosis of TDC and has an important role before surgery to rule out complications, and the lesion may be anechoic, homogeneously hypoechoic with intralesional septa, appear pseudo-solid due to possible protein contents or heterogeneous [10]. However, USI was not able to visualize a tract extending towards the tongue base in our case.
The Sistrunk procedure is the surgical treatment of choice. The procedure includes excision of the cyst, thethyroglossal tract, and the central portion of the hyoidbone to prevent recurrence [1].
The epithelial lining of a TGDC ranges from squamous epithelium to pseudostratified ciliated columnar epithelium. Salivary gland tissue or thyroid gland tissue maybe seen in the wall of the cyst [11].
Branchial cleft anomalies may present as a cyst, sinus, fistula, or cartilaginous remnant [12]. Our patient had branchial fistulae, contradicting thus the specialty literature data that show approximately 80% of branchial cleft anomalies present as a cyst andabout 95% are formed from the region of the second branchial arch [13,14].
Although branchial cleft fistulae are congenital andmight be noted at birth, most are not detected until thefirst or second decade of life.
Anatomically, a typical second cleft fistula has its external opening at the anterior border of SCMmuscle at the junction of middle and lower 1/3rd. Second arch anomalies are classified into four types. Type I lesions lie anterior to the sternocleidomastoid muscle SCM and do not come in contact with the carotid sheath. Type II lesions are the most common and pass deep to the SCM and either anterior or posterior to the carotid sheath. Type III lesions pass between the internal and external carotid arteries and are adjacent to the pharynx. Type IV lesions lie medial to the carotid sheath close to the pharynx adjacent to the tonsillar fossa [15]. Our case had the type II pattern.
Clinically symptoms consist of intermittent or continuous mucous discharge from the anterior aspect of neck. In addition presence of infection may leads to formation of an abscess and signs of inflammationat the site of opening. The diagnosis is established by physical examination and radiological investigations are rarely asked for. However, a fistula gram if performed delineates the tract and it is often the common investigation available [16].This paraclinical exploration didn’t practice to this patient.
The definite treatment of branchial anomalies is complete surgical excision of tract, most suitable age for surgery is 2 to 3 year or as early as possible if it is already delayed and among surgical techniques stepladder incision is most accepted method [17]. The reported incidence of recurrence rate was 3% where only external approach was used. The studied patient was performed complete excision of fistulous tract and as a proof stands the absence of recurrence within 1 year.
In conclusion, our case showed that there is a possibility that more than one anomaly can be seen in same patient simultaneously, so that we should always keep in mind and look for a possible associated or concurrent lesion in any case of head and neck sinus or fistula. Which though very rare is, but a reality and little alertness and simple management can prevent unwanted second surgeries.
 |
| Figure 1: Intraoperative picture showing the coexistence of a A) thyroglossal duct cyst and B) fistula of the second branchial cleft |
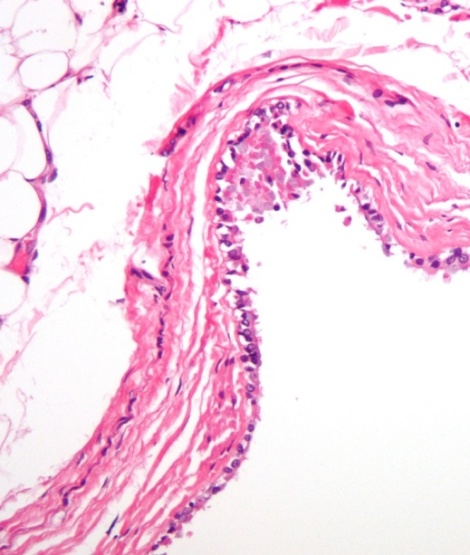 |
| Figure 2: Thyroglossal duct histology |
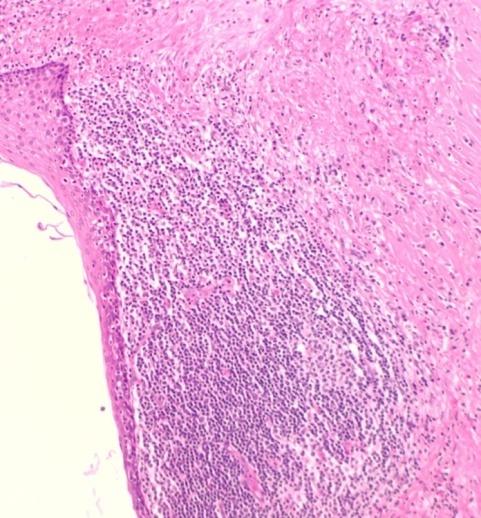 |
| Figure 3: Branchial fistulae histology |






































