Top Links
Clinical and Experimental Research in Cardiology
ISSN: 2394-6504
Atorvastatin prescription before and after Percutaneous Coronary Intervention: Effects on Left Ventricular Ejection Fraction and blood circulating Pentraxin3
Copyright: © 2015 Namazi MH. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Related article at Pubmed, Google Scholar
Introduction: Statins can reduce risk of myocardial infarction, stroke and mortality in high risk individuals and improve clinical outcomes in patients undergoing Percutaneous Coronary Intervention (PCI). The major challenge of physicians at the emergency condition is the fact that patients are not stable and cannot take several pills, wholesale.
Methods: This study was carried out on 100 patients who suffered from AMI with the early plan for primary PCI. All patients were divided to two group, randomly; fifty patients received conventional drug including Atorvastatin (80 mg/day), Aspirin (325 mg/day) and Clopidogrel (600 mg/day) at the time of admitting to the emergency and before primary-PCI; the other 50 patients take same drug regime without Atorvastatin just like the control group, before primary-PCI and a single dose Atorvastatin (80 mg/day) after primary PCI. A paired T-test was employed to study the result of PTX3 and LVEF before and after primary PCI among all patients. An independent T-test was also used for statistical analysis of the result of PTX3 value and EF after primary PCI for both drug plan intervention groups.
Results: PTX3 and LVEF values in the group with Atorvastatin pre-treatment changed from 6.07 ± 2.31 ng/dL to 4.92 ± 1.98 ng/ dL and 40.8 ± 8.88 to 45 ± 6.77, respectively after primary PCI. Both mentioned indexes in the Atorvastatin post-treatment group were also changed from 5.91 ± 3.24 ng/dL to 5.37 ± 3.6 and 41.2 ± 8.66 to 44.9 ± 7.79, respectively, after primary PCI. None statistically significant difference were seen in comparison the results of both LVEF (P value = 0.946) and PTX3 (0.445) values between two groups.
Conclusion: Our results indicate that Atorvastatin therapy after primary-PCI may has same beneficial effects on Cardiac functions compared with conventional drug regime before PCI.
Keywords: PCI; Atorvastatin; Ejection Fraction; Pentraxin3Coronary Artery Diseases (CAD) is one of the most prevalent causative agents of morbidity and mortality, worldwide [1]. Many studies have been reported the role of statins that not only reduce risk of myocardial infarction, stroke and mortality in high risk individuals but also improve clinical outcomes among patients undergoing Percutaneous Coronary Intervention (PCI) [2] for stable coronary artery diseases and non-ST segment elevation coronary syndrome [3,4] as well as ST segment elevation myocardial infarction [5].
At the time of PCI, Periprocedural myocardial injury is associated with more complication events [6] and therefore reducing the adverse events is one of the main goals. Previous studies showed that pre-treatment with statins before PCI can reduce cardiovascular complications after PCI [7,8,4]. Some studies suggest that statin therapy is able to stabilize coronary plague, decrease the chance of thrombus formation and increase endothelial function [9]. However, the major challenge of physicians at the emergency condition is the fact that the patients are not stable and cannot take several pills (Atorvastatin, Aspirin and Clopidogrel), wholesale. In the other hand, although as mentioned above, almost all clinical trials have reported the efficacy of Atorvastatin pre-treatment of patients undergoing PCI but there are only few studies about Atorvastatin post-treatment of patients after PCI [10].
PTX3 is a new interesting inflammatory indicator that has homology in both structure and function with hs-CRP (highly sensitive C Reactive Protein) [11]. Compared with hs-CRP, this indicator has more specificity role in diagnosis of Coronary Artery Diseases [12,13]. Indeed, several studies have showed correlation between PTX3 with CAD and Syntax score [14,15].
Therefore we aimed to survey the effects of Atorvastatin treatment beside Aspirin and Clopidogrel as conventional therapy before primary PCI with a drug plan as prescribing Aspirin and Clopidogrel before PCI and then a single dose of Atorvastatin (80 mg/day) after primary PCI on Pentraxin3 (PTX3) and Left Ventricular Ejection Fraction (LVEF) in patients who suffer from Acute Myocardial Infarction (AMI) with an early plan for primary PCI.
This study was carried out on patients who seeking care from a general hospital (Moddarres Hospital), department of Cardiology, during 2013-2014. For describing AMI, patients who had ST Elevation in ECG leads beside positive troponin or acute and typical chest pain were diagnosed as AMI and underwent primary PCI up to 1 hours after admitting to the hospital.
All patients with prinzmetal angina, pulmonary edema, cardiogenic shock, high blood pressure, and previous history of consuming Atorvastatin were excluded from the study.
A total 100 patients who suffered from AMI with the early plan for primary PCI were enrolled in this study. All patients who were included in the study rested for 15 min in the sitting position and then blood pressure was taken using a standardized mercury sphygmomanometer. A same physician performed primary PCI and a trained interviewer also filled questionnaires consisted of demographic data, smoking status and history of medical situation using face to face model.
when patients enrolled for the study, they were divided to two equal groups using double blind method, randomly; a control group including 50 patients who received conventional drug regime including 80 mg/day Atorvastatin, 325 mg/day Aspirin and 600 mg/day Clopidogrel at the time of admitting to the emergency, before primary PCI and the other 50 patients take same drug regime without Atorvastatin at the same time. The latter group received Atorvastatin 80 mg/day post-treatment after primary PCI; 24 hours after admitting to the hospital. At the time of enrolling patients in the study and before primary PCI, LVEF and PTX3 levels were assessed. For the second time, evaluation of PTX3 and LVEF was also performed for all enrolled patients 24 hours and 5 days after admitting to the hospital, respectively.
The same technician using commercial Human Pentraxin-3 ELISA kit (CUSABIO BIOTECH CO., Japan) according to the previous study [16] evaluated PTX3 value. Same persons performed all evaluations on PTX3 levels and LVEF.
Gathered data was analyzed using SPSS version 22 for windows. Descriptive data for continuous variable for normal and non-normal distribution was presented as Mean (SD) and median (IQR), respectively. Categorically distributed variables were also described as frequency (n,%). A paired T-test was employed to study the result of PTX3 and LVEF before and after PCI among patients of both groups. An independent T-test was also used for statistical analysis of the result of PTX3 value and LVEF after PCI for both drug plan intervention groups. P-value less than 0.05 considered as significant in all analysis.
All patients who were enrolled in this study were aware about the study as well as drug regime changes and all experiments on the patients were performed based on guidelines of the ethical board of Shahid Beheshti University of Medical Sciences.
The age mean ± SD and man/woman percent of all patients who participated in our study were 59.28 ± 10.29 and 84/16 percent, respectively. The demographic data was summarized in Table 1. Statistically significant changes were observed in all patients who enrolled in the study. The employed paired T-test in both groups showed that primary PCI in both drug regime groups including Atorvastatin 80 mg/day, before or after primary PCI, improved PTX3 and LVEF values. PTX3 and LVEF values in group with Atorvastatin pre-treatment changed after primary PCI, from 6.07 ± 2.31 ng/dL to 4.92 ± 1.98 ng/ dL and 40.8 ± 8.88 to 45 ± 6.77, respectively. Both mentioned indexes in the Atorvastatin post-treatment group were also changed after Primary PCI, from 5.91 ± 3.24 ng/dL to 5.37 ± 3.6 and 41.2 ± 8.66 to 44.9 ± 7.79, respectively. Also the vital capacity of the patients in two groups dramatically increased (Figure 1,2).
An Independent paired T-test showed that there is not statistically significant difference in the results of both LVEF (P value = 0.946) and PTX3 (0.445) values in comparison between two groups.
In this study, we showed that prescribing common dose of Aspirin and Clopidogrel before and high-dose of Atorvastatin (80 mg/day) after primary PCI has the same results compared with conventional therapy including Atorvastatin pre-treatment beside Aspirin and Clopidogrel just before primary PCI.
In recent years, the numbers of studies that describe beneficial effects of statins on PCI outcome and lowering the blood lipid have dramatically increased. The beneficial effects of statins in heart failures and improving the life quality and quantity of patients with AMI have well known by several randomized studies [17-21]. Previous studies showed promising effects of Atorvastatin pre-treatment before PCI on expanding the lifetime as well as reducing perprocedural MI of patients during a long-term fallow up [3,7,22]. Lev and colleagues illustrated that statin pre-treatment effect on micro vascular functions and so, this event may improve coronary blood flow, after PCI [23]. Beneficial effects of statins are likely more than only lowering the blood lipid. As mentioned heretofore, statins can improve the endothelial function [24] and act as an anti- inflammatory agent [25,26], coronary microvascular dilator [27], as well as antithrombotic factor [28].
Several studies have demonstrated the beneficial effects of Atorvastatin pre-treatment before PCI but after the literature review, we could find just few studies about the efficacy of Atorvastatin post-treatment after PCI. Kuei and colleagues described that although Atorvastatin after PCI had a negative effect on Adiponectin system, anti-inflammatory and anti-atherogenic properties, but positive effects of Atorvastatin post- treatment after PCI on patients could frustrate the negative ones that mentioned [10]. Our compared results between two groups of our study is in agreement with mentioned study that showed the beneficial effects of Atorvastatin post-treatment, after a primary PCI.
In our study, LVEF as a vital capacity of the patients was significantly improved in both groups; from 40.8 ± 8.88 to 45 ± 6.77 in group with conventional drug regime and from 41.2 ± 8.66 to 44.9 ± 7.79 in the group with Atorvastatin post-treatment. The result of the study is in consistent with previous studies. Node et al showed that statin therapy for 3 months decreased left ventricular end-systolic volume in patients with idiopathic dilated cardiomyopathy [29]. In the other study, Teshima and colleagues demonstrated that Atorvastatin therapy early after an AMI onset improved LVEF [30]. Our study also showed that the results in both group are same. This finding illustrates that a single dose of Atorvastatin (80 mg/day) after primary PCI can also have beneficial effect on cardiac functions just like the conventional drug plan.
PTX3 has known as a multifunctional conserved protein like C-Reaction Protein (CRP) that both of them are blood inflammatory indicators [31,32]. Although there are several studies that described the relationship between CRP, as an inflammatory indicator, and Atorvastatin [33-35], but we believe that the current study is one of the first human study that shows the effects of Atorvastatin therapy before and after primary PCI on PTX3. Our findings revealed that Atorvastatin treatment before or after primary PCI decreased the blood PTX3 values. As mentioned in the results, Atorvastatin pre and post-PCI treatment attenuated the plasma levels of PTX3. This finding may be related to anti-inflammatory effect of Atorvastatin that reduced the plasma levels of an inflammatory indicator, blood-circulating PTX3.
Our study had some limitations. The most important limitation of this study was enrolling patients in the study. Most of patients did not accept enrolling in our study, so samples achieving was a challenge. The authors believe that next studies on greater sample size will reveal results that are more interesting.
Our results indicate that Atorvastatin therapy after PCI, particularly in the emergency conditions that the patient is not stable and cannot take several pills, has the same beneficial effects on Cardiac functions compared with conventional drug regime before PCI.
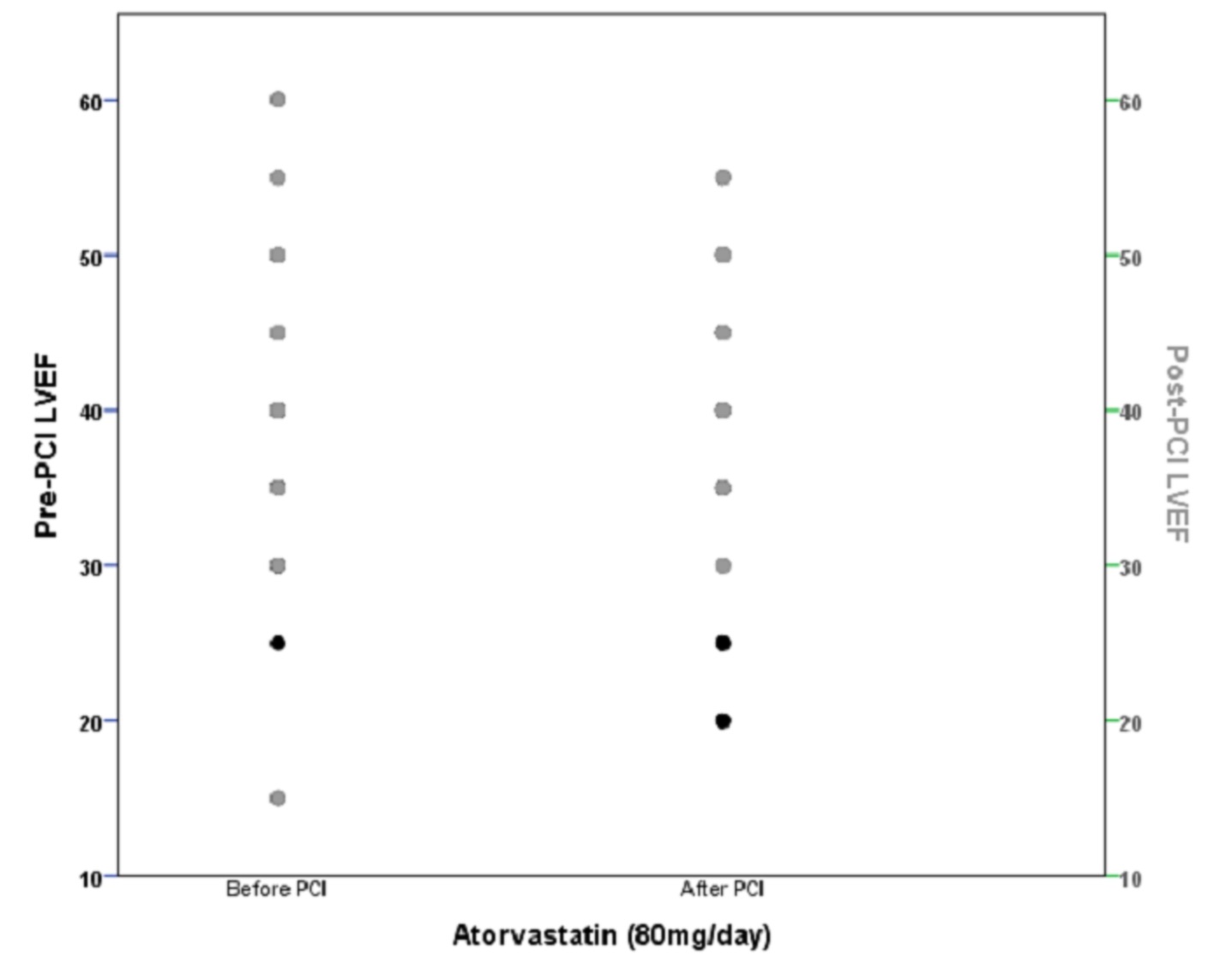 |
| Figure 1: significant change of LVEF in both Atorvastatin pre and post –PCI treatment (p= 0.000) and statistically non-significant change of LVEF between two groups (p=0.946) at the end of study; LVEF: Left Ventricular Ejection Fraction, PCI: Percutaneous Coronary Intervention |
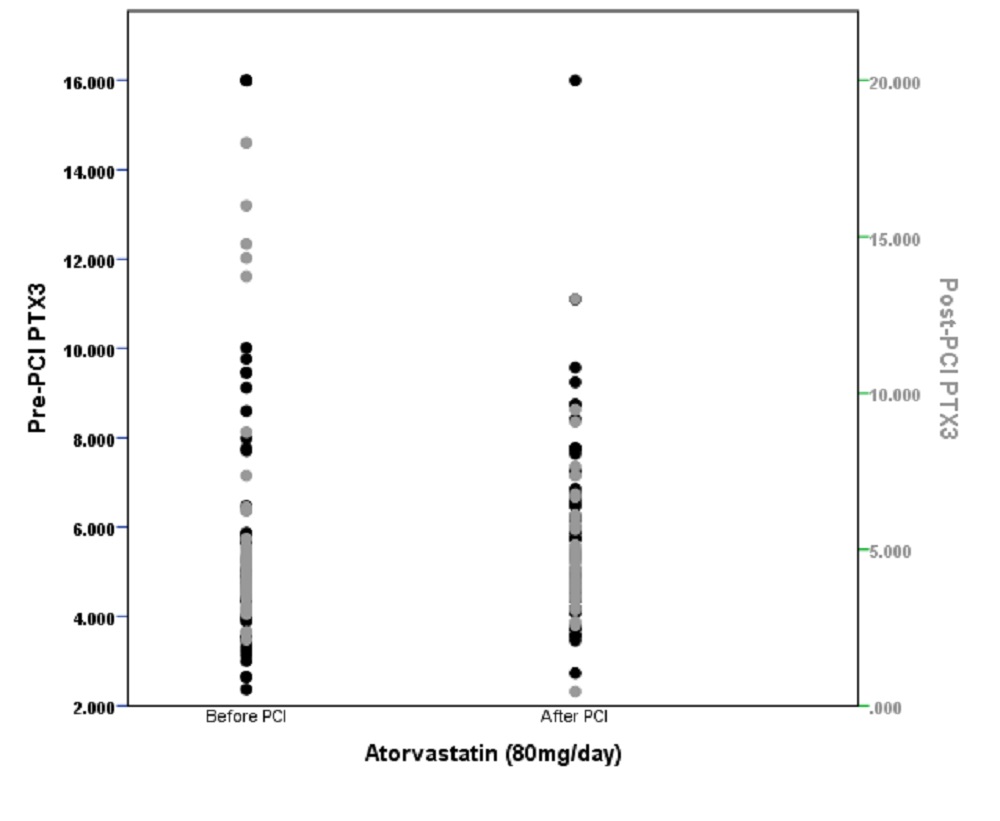 |
| Figure 2: significant change of plasma PTX3 levels in both Atorvastatin pre and post-PCI treatment (p=0.043) and statistically non-significant change of PTX3 between two groups (p=0.445) at the end of study; PTX3: Pentraxin 3, PCI: Percutaneous Coronary Intervention |
| Male/female (%) | 84/16 |
| Age (year) | 59.28 ± 10.29 |
| Smokers (%) | 46% |
| Triglyceride (mg/ L-1) | 154.6 ± 82.05 |
| Diabetes Mellitus (%) | 25% |
| Hypertension (%) | 27% |
| High-density Lipoprotein cholesterol (mg/L-1) | 45.18 ± 13.08 |
| Low- density Lipoprotein cholesterol (mg/L-1) | 104.18 ± 33.16 |
| Data are presented as number (%) or mean Table 1: Demographic data of the patients participated in this study |
|






































